| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website http://www.theijcp.org |
Case Report
Volume 2, Number 1, June 2013, pages 37-39
Acute Cystitis in a Patient With Kawasaki Disease
Toru Watanabe
Department of Pediatrics, Niigata City General Hospital, 463-7 Shumoku, Chuo-ku, Niigata City 950-1197, Japan
Manuscript accepted for publication May 24, 2013
Short title: Acute Cystitis
doi: https://doi.org/10.4021/ijcp102w
| Abstract | ▴Top |
Kidney and urinary tract involvement has been well described in patients with Kawasaki disease (KD). Sterile pyuria is the most common abnormal finding in patients with KD who have kidney and urinary tract involvement. Although pyuria can also originate from the bladder, cystitis has rarely been reported in patients with KD. We described here a case of acute cystitis in a patient with KD. A 5-year-old boy with KD had abdominal pain, miction pain and sterile pyuria. A computed tomography of the abdomen showed diffuse thickening of the urinary bladder, which was compatible with a diagnosis of acute cystitis. Intravenous immunoglobulin therapy rapidly improved the signs of KD and miction pain. Healthcare providers should be aware of acute cystitis as a complication of KD if patients have pyuria and/or bladder symptoms.
Keywords: Urinary tract; Pyuria; Urinary bladder; Complications; Kawasaki disease
| Introduction | ▴Top |
Kawasaki disease (KD) is an acute febrile vasculitis that predominantly affects children ≤ 5 years of age [1]. Because KD is a systemic vasculitis, multiple organ involvement can develop, including coronary artery lesions, carditis, arthritis, hepatitis, gastrointestinal complications, central nervous system disease [2, 3], KD shock syndrome [4], hyponatremia [5], and kidney and urinary tract involvement [6]. Sterile pyuria is the most common abnormal finding in patients with kidney and urinary tract involvement [6]. Although pyuria can also originate from the bladder, cystitis has rarely been reported in patients with KD [7]. This report describes acute cystitis in a patient with KD.
| Case Report | ▴Top |
A previously healthy, 5-year-old Japanese boy was admitted to our hospital for evaluation of a 3-day history of high-grade fever, left cervical lymph node swelling, exanthema on the trunk, abdominal pain, diarrhea, vomiting, and miction pain. At the time of admission, a physical examination revealed bilateral conjunctivitis, erythema of the lips and oral mucosa, left cervical lymph node swelling (2 × 3 cm), a polymorphic truncal rash, abdominal distension, and abdominal tenderness without guarding. His vital signs were as follows: body temperature, 40.4 °C; blood pressure, 89/59 mmHg; and pulse rate 132 beats/min. Laboratory studies revealed leukocytosis (white blood cell count, 16,900/µL), elevated C-reactive protein (CRP; 10.43 mg/dL; reference range, 0.01 - 0.31 mg/dL), increased levels of aspartate aminotransferase (AST; 402 IU/L; reference range, 11 - 31 IU/L), alanine aminotransferase (ALT; 415 IU/L; reference range, 7 - 42 IU/L) and total bilirubin (2.8 mg/dL; reference range, 0.2 - 1.2 mg/dL), and hyponatremia (sodium, 131 mEq/L). Serum potassium, chloride, creatinine, uric acid, and blood urea nitrogen levels were all normal. Serum IgG, IgA, IgM, C3, C4 and CH50 levels and the anti-streptolysin O titer were within normal ranges. Serologic tests for antinuclear antibody, hepatitis B virus surface antigen, and anti-hepatitis C virus antibody were negative. Urinalysis showed 2 + protein, 2 + bilirubin, 1 + occult blood, and 10 - 19 red blood cells and > 100 white blood cells per high-power field. The urinary protein to creatinine ratio was 1.37 g/g creatinine. The urinary β2-microglobulin concentration was 12.45 mg/L (normal < 0.15 mg/L). Bacterial and viral urine culture grew no pathogens and the urinary polymerase chain reaction test for adenovirus was negative. An abdominal radiograph showed a large amount of gas distributed throughout the large intestine. A post-contrast computed tomography of the abdomen, performed to rule out intestinal obstruction, showed diffuse thickening of the urinary bladder wall (Fig. 1) and a large amount of gas distributed throughout the large intestine. An abdominal ultrasound also showed thickening of the urinary bladder wall (Fig. 2).
 Click for large image | Figure 1. Post-contrast computed tomography of the abdomen showing diffuse thickening of the urinary bladder wall. |
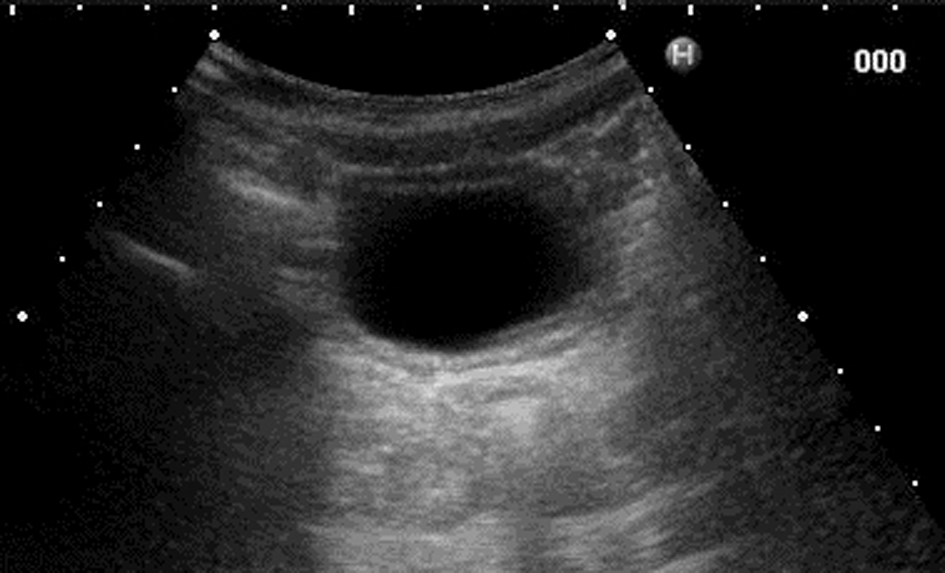 Click for large image | Figure 2. Abdominal ultrasound also showing thickening of the urinary bladder wall. |
The patient was diagnosed with incomplete KD, had acute cystitis, renal involvement and paralytic ileus, and underwent intravenous immunoglobulin therapy (IVIG; 2 g/kg/dose) for 1 day and oral administration of flurbiprofen (4 mg/kg per day). Because the patient remained febrile 2 days later, he was diagnosed with complete KD. The second dose of IVIG resulted in rapid improvement of the KD signs and dysuria. Liver function tests, complete blood cell count, CRP level and urinary β2-microglobulin concentration returned to normal ranges, and urinalysis showed no abnormal findings 10 days after admission. An echocardiogram was normal and the urinary bladder was normal on the follow-up abdominal ultrasound 4 weeks after the onset of the present illness.
| Discussion | ▴Top |
Our patient with KD developed acute cystitis. Kidney and urinary tract involvement has been well described in KD and has included interstitial nephritis, acute renal failure, hemolytic uremic syndrome, nephrotic syndrome and abnormal urinary findings such as proteinuria, hematuria or pyuria [5]. Pyuria is the most common abnormal urinary findings in patients with KD, and is considered to originate from the urethra and/or the kidney as a result of mild and subclinical renal injury [6]. Pyuria can also originate from the bladder due to cystitis; however, only one necropsy study has shown cystitis in patients with KD [7]. Amano and colleagues studied 37 autopsied patients with KD and reported that several patients with KD had cystitis [7]. The authors did not provide detailed histologic findings or possible mechanisms underlying cystitis in patients with KD.
Cystitis has been reported in primary vasculitis other than KD. Pery et al [8] examined eight patients with Henoch-Schonlein purpura (HSP) using abdominal ultrasonography and revealed that two patients with macroscopic hematuria had marked and diffuse mucosal thickening of the urinary bladder, which confirmed the diagnosis of hemorrhagic cystitis as a part of HSP. Allen et al [9] described a 4-year-old girl with HSP who developed hemorrhagic cystitis detected by ultrasonography. Block [10] reported a 57-year-old woman with non-granulomatous necrotizing vasculitis who developed hemorrhagic cystitis that was confirmed by cystoscopy. Pathological examination of biopsy specimens from the bladder wall revealed fibrinoid necrosis of the blood vessel walls, with leukocytic infiltration.
Cystitis has also been reported in patients with systemic lupus erythematosus (SLE) and secondary vasculitis, termed lupus cystitis [11]. Lupus cystitis is characterized by small volume urinary frequency and is often associated with gastrointestinal symptoms [11]. Histologically, lupus cystitis is an interstitial cystitis characterized by mononuclear cell infiltrate and edema in the interstitium of the urinary bladder [12]. Because some patients with lupus cystitis have immunofluorescent deposits in the blood vessel walls of the urinary bladder, lupus cystitis is suggested to be caused by immune complex-mediated vasculitis secondary to SLE [13].
The precise pathogenic mechanism underlying the development of acute cystitis in our patient with KD is unclear because our patient did not undergo histologic examination of the urinary bladder; however, it appears likely that vasculitis of the bladder as a part of KD caused cystitis in our patient because bacterial and viral urine cultures did not grow any pathogens, dysuria promptly improved after IVIG therapy, and the thickening of the urinary bladder wall resolved following disappearance of KD signs and laboratory inflammatory findings. Healthcare providers should be aware of acute cystitis as a complication of KD if patients have pyuria and/or bladder symptoms.
In summary, we described a patient with KD who developed acute cystitis that resolved following IVIG therapy. The precise pathogenic mechanism underlying acute cystitis in our patient is unclear. Healthcare providers should be aware of acute cystitis as a complication of KD.
Conflict of Interest
The author declares no potential conflict of interests.
| References | ▴Top |
- Kawasaki T, Kosaki F, Okawa S, Shigematsu I, Yanagawa H. A new infantile acute febrile mucocutaneous lymph node syndrome (MLNS) prevailing in Japan. Pediatrics. 1974;54(3):271-276.
pubmed - Burns JC. Kawasaki disease. Adv Pediatr. 2001;48:157-177.
pubmed - Tizard EJ. Complications of Kawasaki disease. Curr Paediatr. 2005;15(1):62-68.
doi - Kanegaye JT, Wilder MS, Molkara D, Frazer JR, Pancheri J, Tremoulet AH, Watson VE, et al. Recognition of a Kawasaki disease shock syndrome. Pediatrics. 2009;123(5):e783-789.
doi pubmed - Watanabe T, Abe Y, Sato S, Uehara Y, Ikeno K, Abe T. Hyponatremia in Kawasaki disease. Pediatr Nephrol. 2006;21(6):778-781.
doi pubmed - Watanabe T, Abe Y, Sato S, Uehara Y, Ikeno K, Abe T. Sterile pyuria in patients with Kawasaki disease originates from both the urethra and the kidney. Pediatr Nephrol. 2007;22(7):987-991.
doi pubmed - Amano S, Hazama F, Kubagawa H, Tasaka K, Haebara H, Hamashima Y. General pathology of Kawasaki disease. On the morphological alterations corresponding to the clinical manifestations. Acta Pathol Jpn. 1980;30(5):681-694.
pubmed - Pery M, Alon U, Lachter JH, Kaftori JK, Gaitini D, Rosenberger A. The value of ultrasound in Schoenlein-Henoch purpura. Eur J Pediatr. 1990;150(2):92-94.
doi pubmed - Allen SJ, Sprigg A, Davidson DC. Haemorrhagic cystitis and urinary retention in Henoch-Schonlein purpura. Eur J Pediatr. 1992;151(4):312.
doi pubmed - Block JA. Hemorrhagic cystitis complicating untreated necrotizing vasculitis. Arthritis Rheum. 1993;36(6):857-859.
doi pubmed - Orth RW, Weisman MH, Cohen AH, Talner LB, Nachtsheim D, Zvaifler NJ. Lupus cystitis: primary bladder manifestations of systemic lupus erythematosus. Ann Intern Med. 1983;98(3):323-326.
doi pubmed - Alarcon-Segovia D, Abud-Mendoza C, Reyes-Gutierrez E, Iglesias-Gamarra A, Diaz-Jouanen E. Involvement of the urinary bladder in systemic lupus erythematosus. A pathologic study. J Rheumatol. 1984;11(2):208-210.
pubmed - Weisman MH, McDanald EC, Wilson CB. Studies of the pathogenesis of interstitial cystitis, obstructive uropathy, and intestinal malabsorption in a patient with systemic lupus erythematosus. Am J Med. 1981;70(4):875-881.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.