Figures
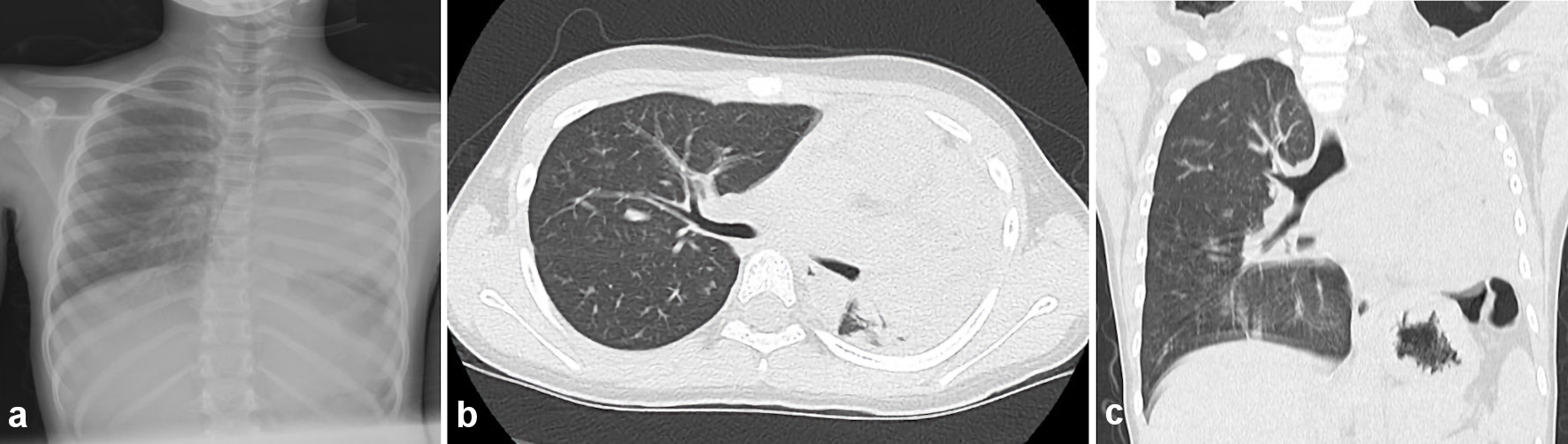
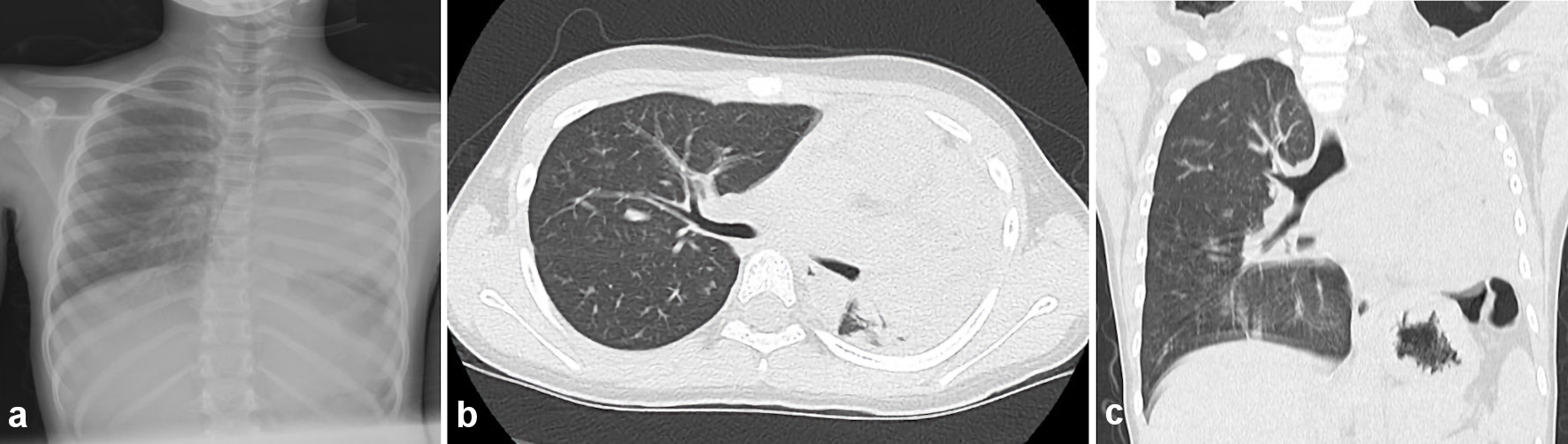
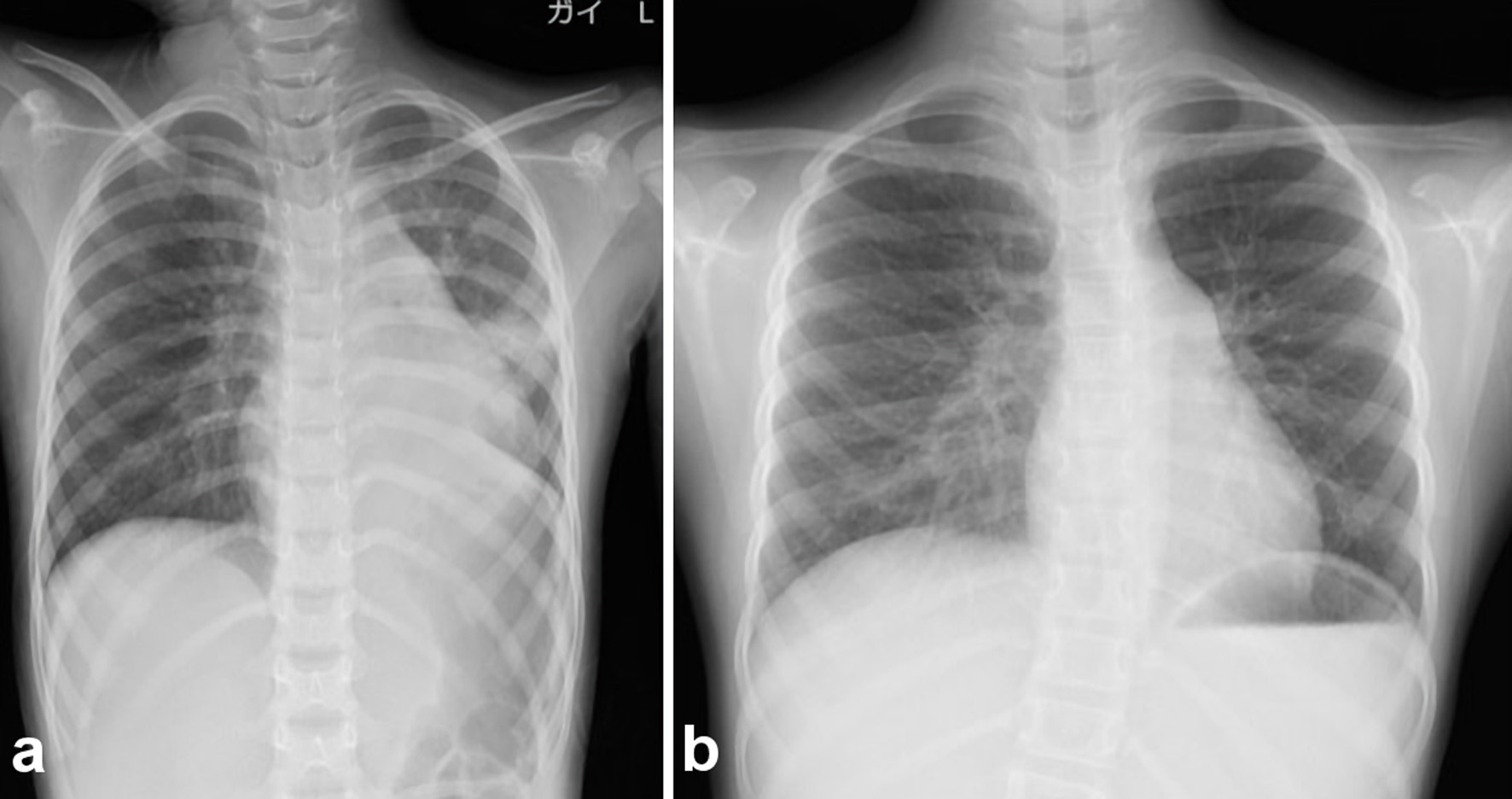
Figure 1. Chest radiography and computed tomography on admission day. (a) Chest radiography on admission revealed the low permeability in the left lung field. (b, c) Chest computed tomography (axial and coronal) revealed the decreasing permeability in the left lung field.
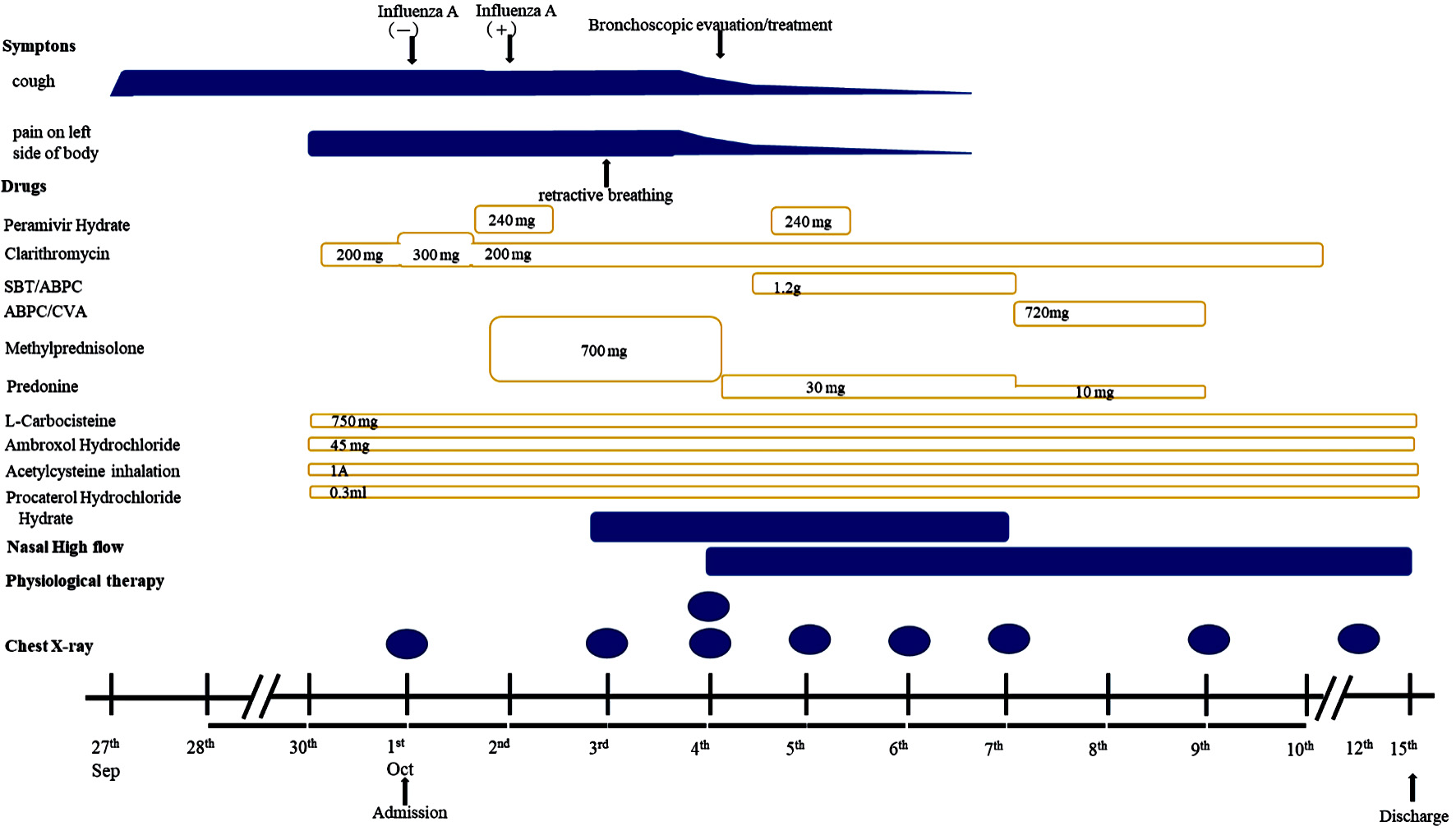
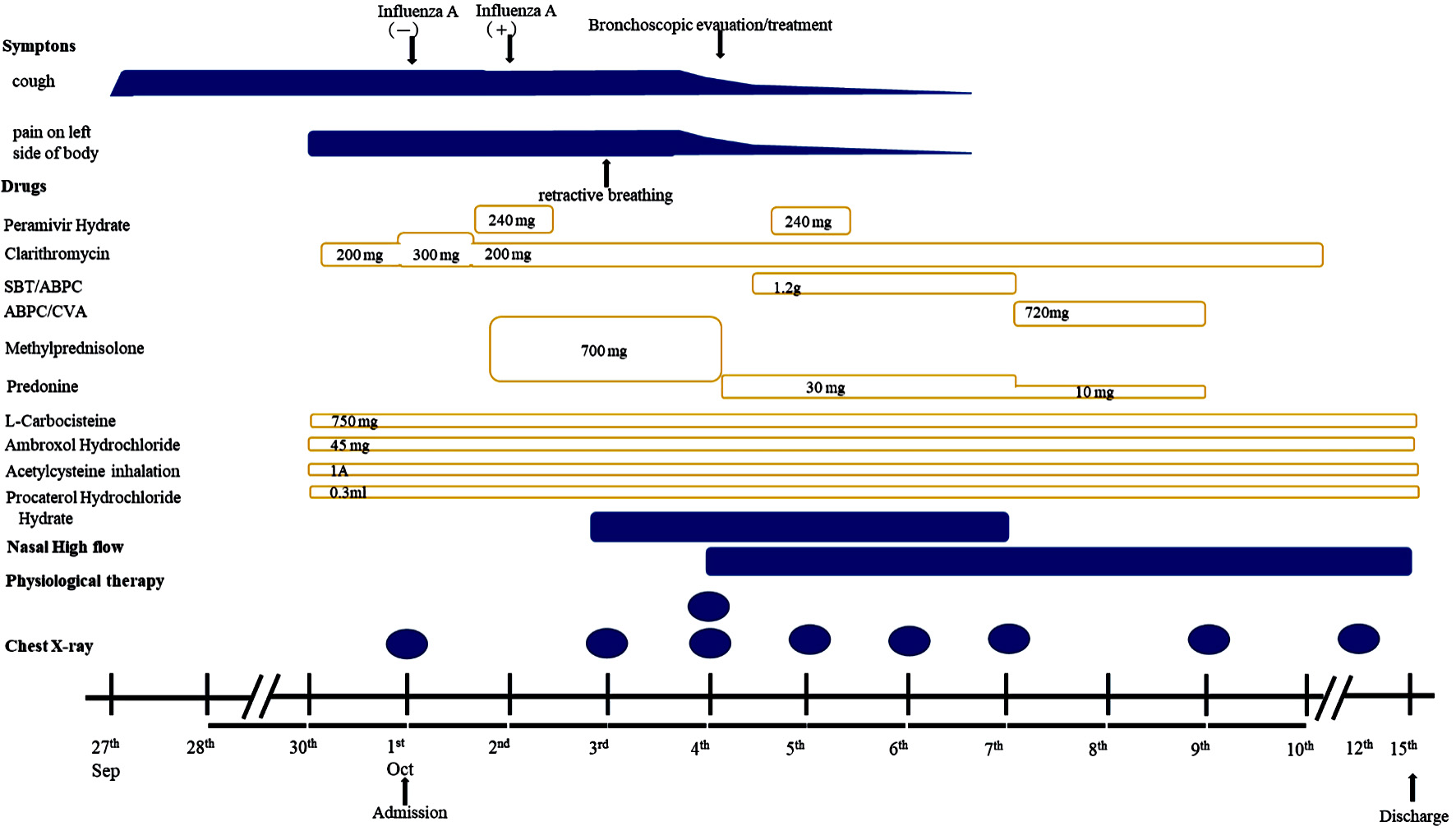
Figure 2. Clinical course after admission. This figure showed time course of applied medicine and chest radiography. SBT/AMPC: sulbactam/ampicillin; AMPC/CVA: amoxicillin-clavulanate.
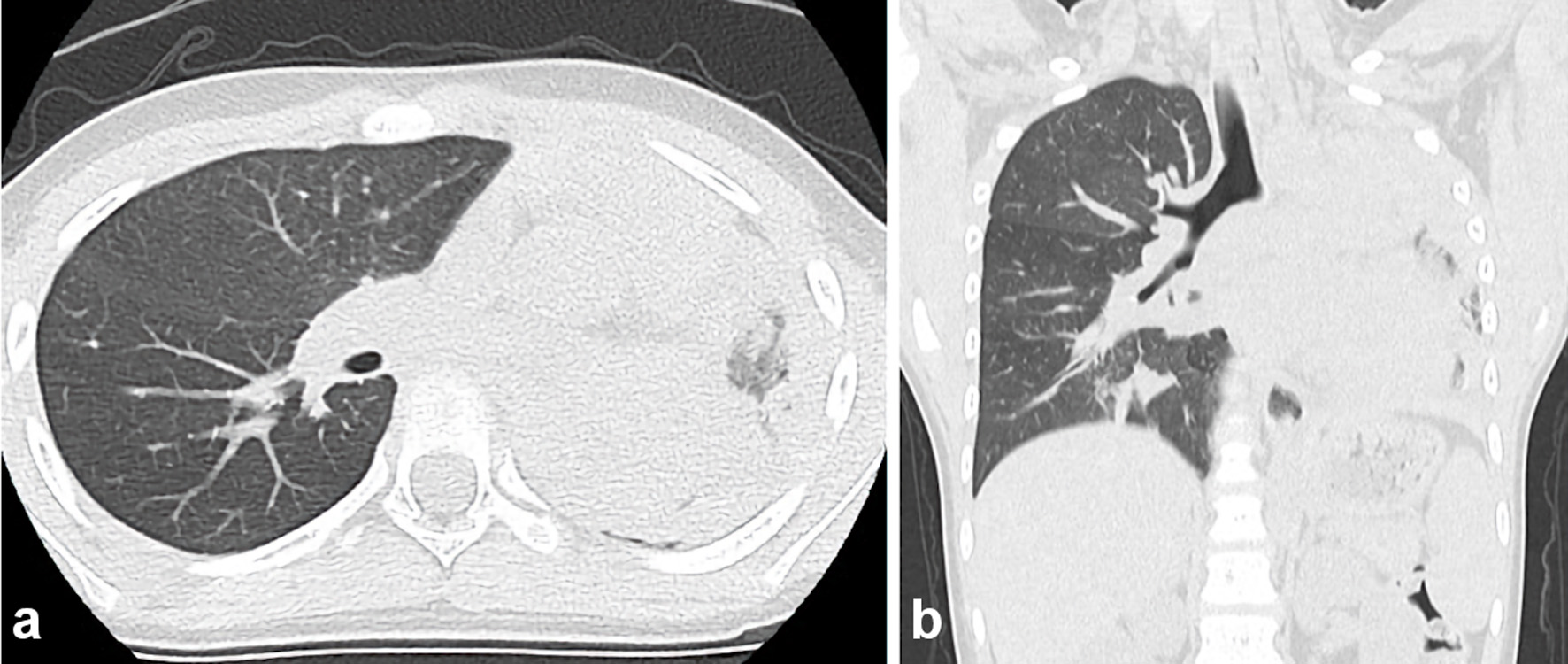
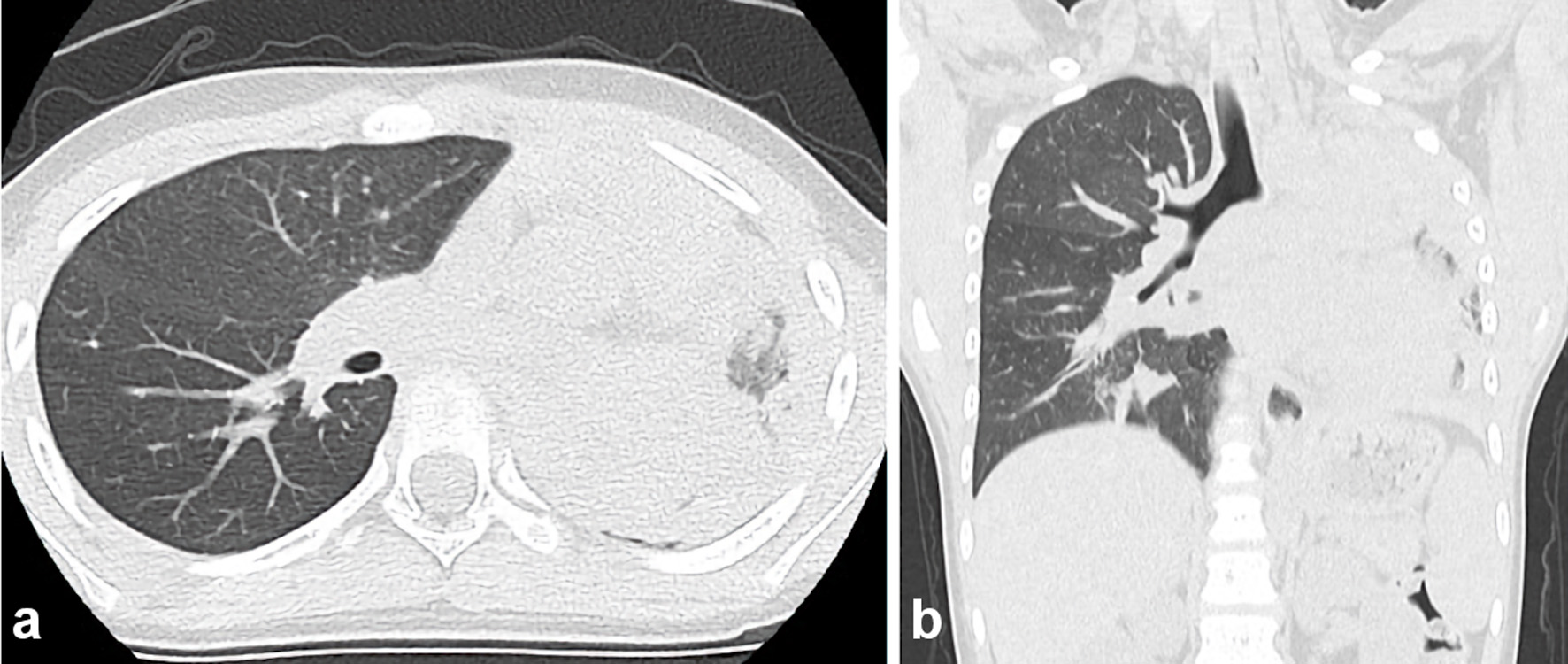
Figure 3. Chest computed tomography on day 4 following admission (axial and coronal) revealing the total atelectasis in the left lung field and a mucous plug in the left bronchus.

Figure 4. (a-f) Bronchoscopic visualization of secretions in the bronchus with patent left lobe orifice. The author (presenter, otolaryngologist) performed flexible bronchoscopy, which revealed a whitish rubbery material occluding the left lower lobe bronchus, and plastic casts were removed. The casts fragmented were removed by extraction via suctioning during fiberoptic bronchoscopy.
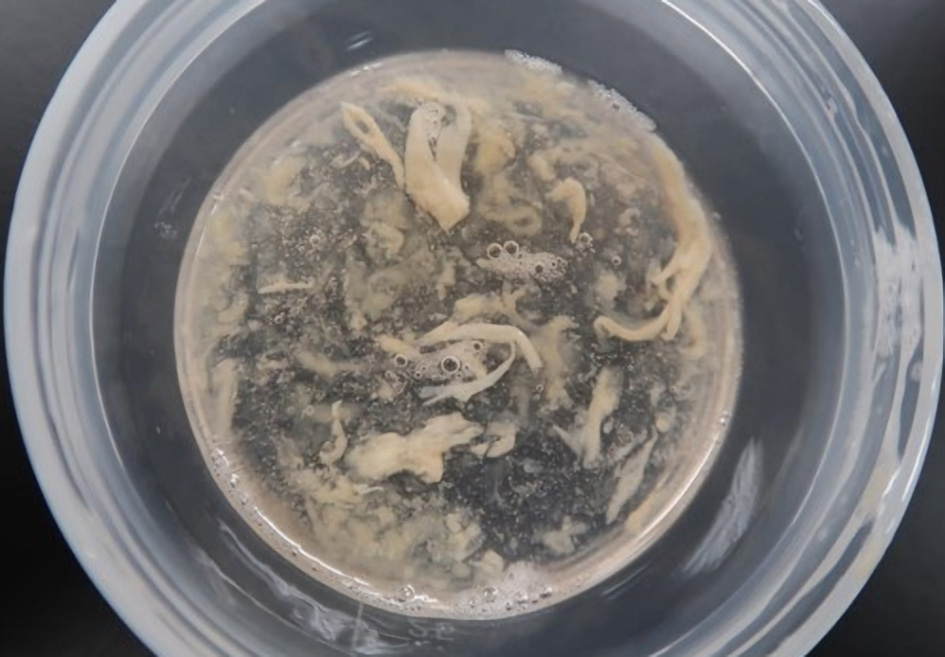
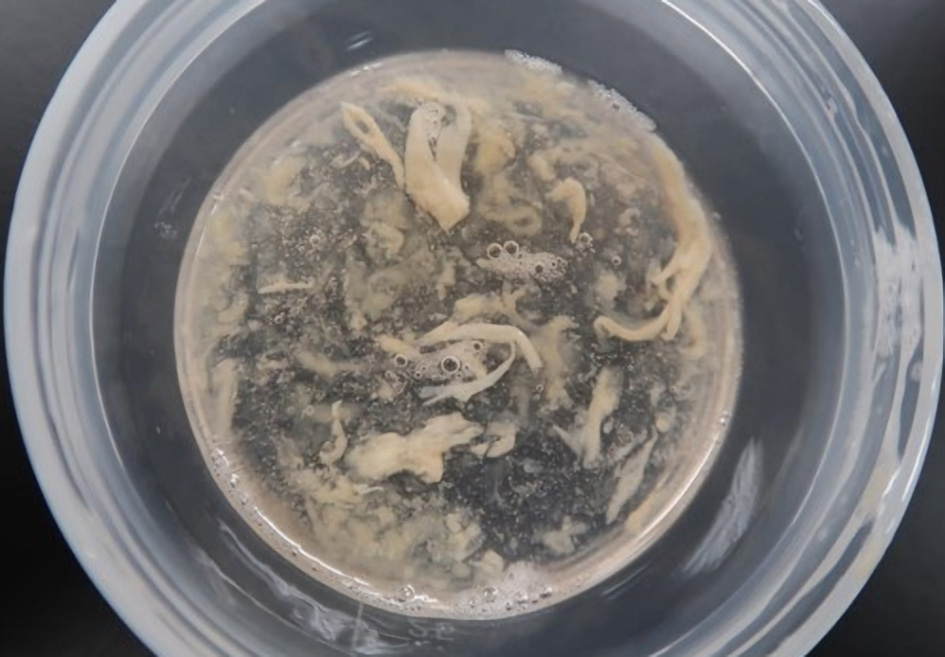
Figure 5. Gross findings demonstrate the fragmentation of casts.
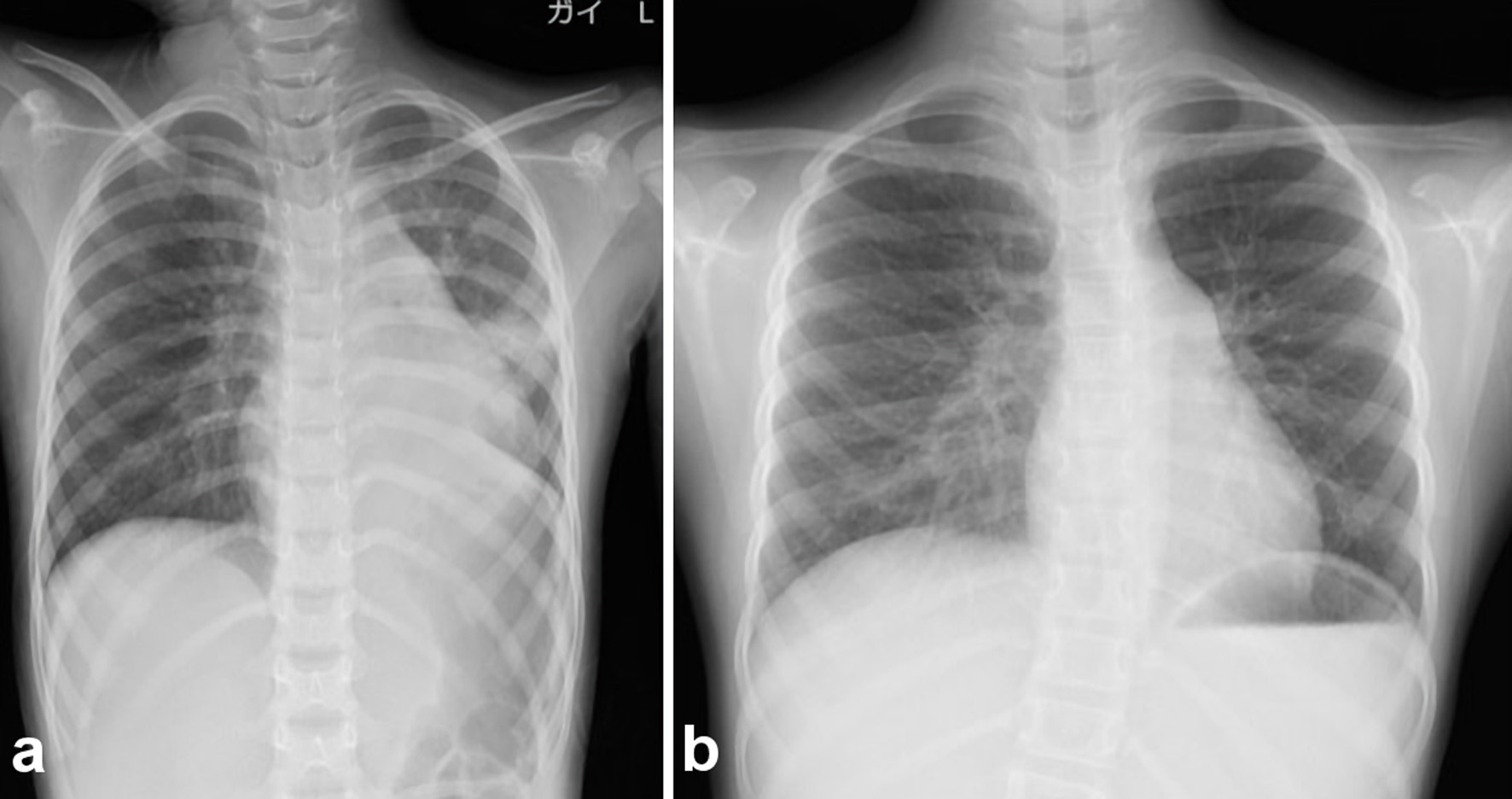
Figure 6. Chest radiography after bronchoscopic suctioning. (a) Finding immediately after bronchoscopic suctioning. After bronchoscopic removal of casts, the atelectasis finding in the left upper lung on chest radiography was improved. (b) Chest radiography revealed a marked improvement in the left lung.
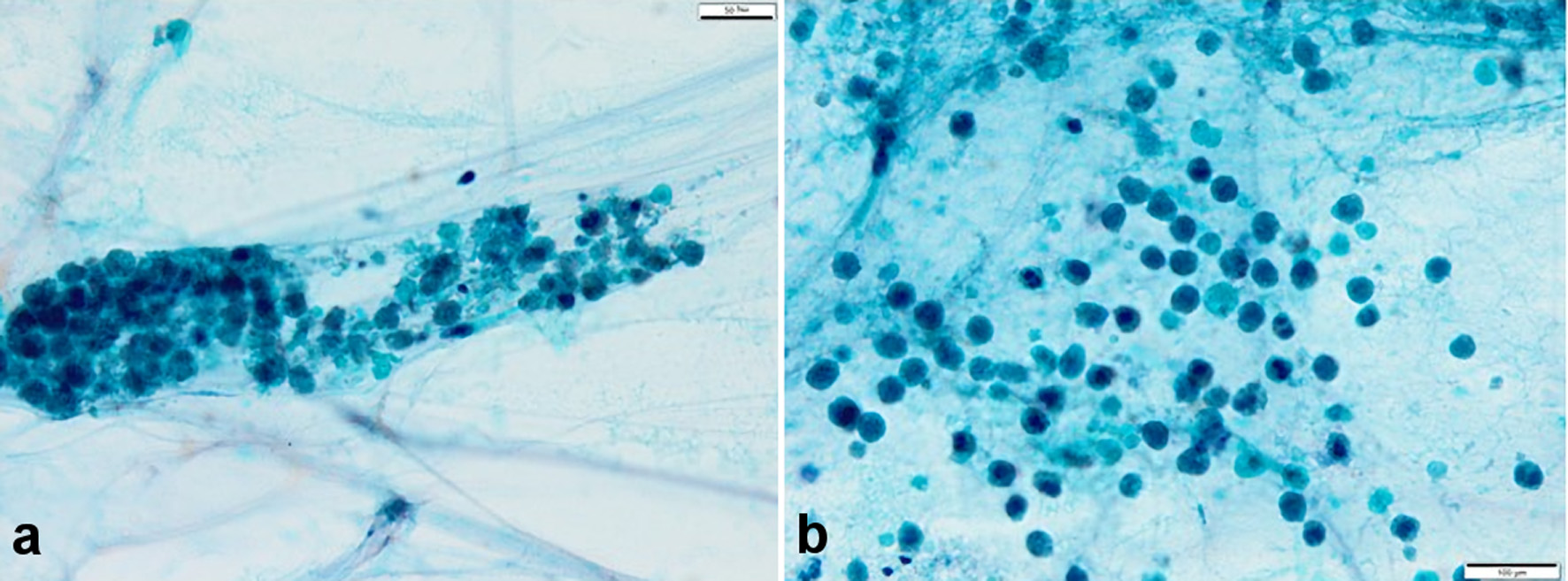
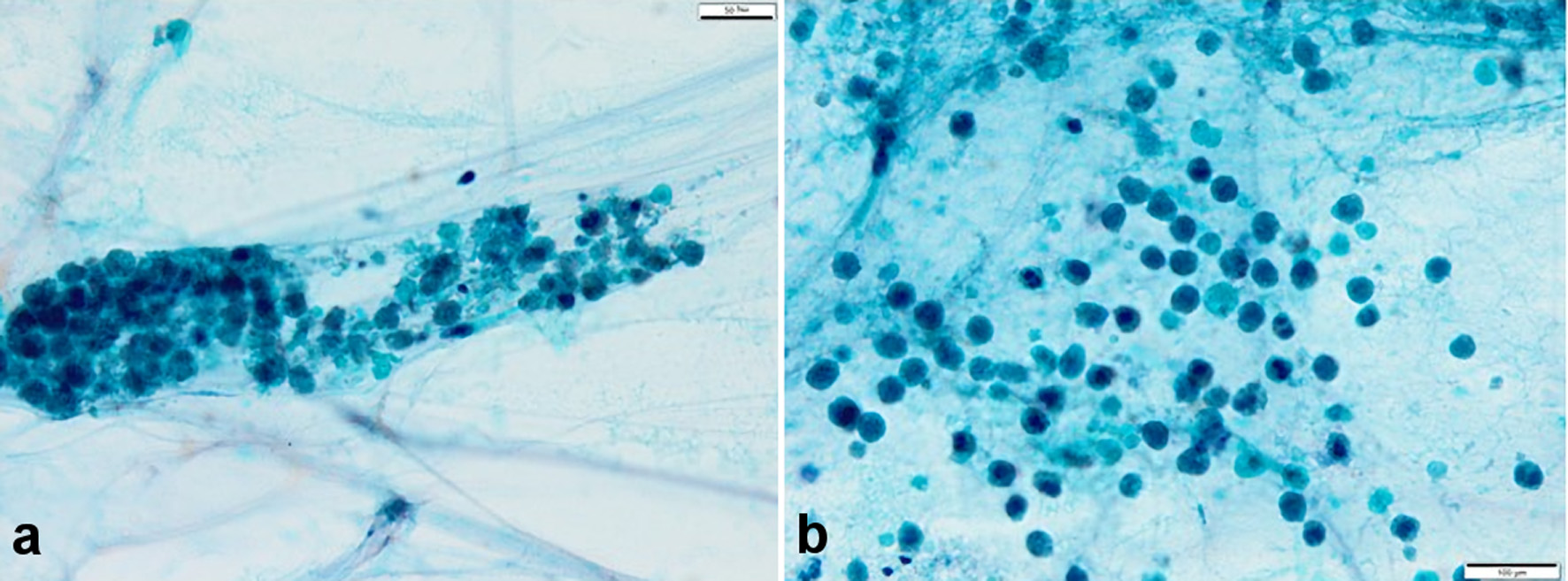
Figure 7. (a, b) Sputum cytopathology (hematoxylin and eosin stain, × 40). Numerous eosinophils were found; however, an evident malignant finding was not found. Eosinophils were considered the inflammatory cells. Charcot-Leyden crystals were not observed.
Tables
Table 1. Laboratory Data on Admission
| aThese are results of October 3 (hospital day 3). WBC: white blood cell; RBC: red blood cell; Hb: hemoglobin; Ht: hematocrit; Plt: platelet; UN: urea nitrogen; Cr: creatinine; TP: total protein; Alb: albumin; TB: total bilirubin; ALT: alanine aminotransferase; AST: aspartate aminotransferase; Ig: immunoglobulin; CRP: C-reactive protein; RSV: respiratory syncytial virus; Flu: influenza virus; IFN: interferon; MG: microglobulin; NAG: N-acetyl-β-D-glucosaminidase. |
| WBC | 8.2 × 103/µL |
| Neutrophils | 79.9% |
| Eosinophils | 1.5% |
| Basophils | 1.2% |
| Lymphocytes | 11.0% |
| RBC | 491 × 104/µL |
| Hb | 13.3 g/dL |
| Ht | 40.0% |
| Plt | 25.8 × 104/µL |
| Na | 139 mmol/L |
| K | 4.3 mmol/L |
| Cl | 105 mmol/L |
| UN | 8.0 mg/dL |
| Cr | 0.23 mg/dL |
| TP | 7.2 g/dL |
| Alb | 4.7 g/dL |
| TB | 0.5 mg/dL |
| AST | 23 IU/L |
| ALT | 11 IU/L |
| IgG | 985 mg/dL |
| IgA | 52 mg/dL |
| IgM | 175 mg/dL |
| CRP | 0.10 mg/dL |
| Non-specific IgE | 209 IU/dL |
| Ferritin | 30 ng/dL |
| RSV | (-) |
| Flu (A/B) | (-/-) |
| Mycoplasma | (-) |
| Cryptococcus | (-) |
| Blood culture | Negative |
| Tuberculosis specific IFN-γ | (-) |
| Urinalysis | |
| Protein | (-) |
| Blood | (-) |
| Sugar | (-) |
| β2-MGa | 260 µg/L |
| NAGa | 46 IU/L |
Table 2. A Total 35 Cases of Pediatric Patients With Influenza Virus-Induced Plastic Bronchitis in Previous English Reports
| Influenza type A | Influenza type B |
|---|
| CT: computed tomography. |
| Case | N = 28 | N = 7 |
| Sex (boy/girl) | 25:3 | 6:1 |
| Age | 1 year and 10 months to 11 years | 5 years to 8 years |
| Average age | 4.4 years | 6.9 years |
| Median age | 4 years | 6 years |
| National | Japanese: 10 | Japanese: 4 |
| Korean: 1 | American: 3 |
| Chinese 17 | |
| Underlying disease (allergy) | 11/28 | 3/7 |
| Affected side on chest X-ray or CT | | |
| Right | 7/28 | 4/7 |
| Left | 9/28 | 3/7 |
| Bilateral | 6/28 | - |
| Unknown | 6/28 | - |
| Therapy | | |
| Antiviral drug | 21/28 | 6/7 |
| Steroid | 19/28 | 5/7 |
| Antibacterial drug | 8/28 | 4/7 |
| Bronchoscopic removal | 28/28 | 7/7 |
| Mechanical ventilation | 25/28 | 6/7 |
| Outcome | 26/28 improve including: 2/28 recurrence (the second attack was infected with influenza type B) improve, 2/28 death | 7/7 improve including: 1/7 recurrence (the second attack was infected with influenza type A) improve |