| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website http://www.theijcp.org |
Case Report
Volume 7, Number 3, September 2018, pages 29-35
Speech and Feeding Improvements in Children After Posterior Tongue-Tie Release: A Case Series
Richard Baxtera, c, Lauren Hughesb
aShelby Pediatric Dentistry, Pelham, AL 35124, USA
bExpressions Center for Communication Disorders, Pelham, AL35124, USA
cCorresponding Author: Richard Baxter, Shelby Pediatric Dentistry, 2490 Pelham Pkwy, Pelham, AL 35124, USA
Manuscript submitted April 25, 2018, accepted June 6, 2018
Short title: Speech and Feeding After Tongue-Tie Release
doi: https://doi.org/10.14740/ijcp295w
| Abstract | ▴Top |
Ankyloglossia, commonly referred to as “tongue-tie,” has recently seen a surge in cases and awareness with a corresponding increase in diagnosis and treatment. The evidence linking tongue-tie release and breastfeeding improvement has been published previously. However, due to a lack of published evidence for children, many medical professionals still believe that a restricted tongue does not contribute to feeding or speech issues in older children. The condition of tongue-tie exists on a continuum with variable visibility and symptoms. Some restrictions, mainly anterior or “classic” tongue-tie, are highly visible and easier to detect. However, “posterior” or submucosal tongue-ties are often more challenging to diagnose. Recently, an increase in awareness and education has led to improved detection of these posterior tongue-ties. The data presented in these case studies will demonstrate that even posterior ties restrict movement and affect oral structures that are required for speech and feeding. In this case series, five patients with posterior tongue restrictions underwent CO2 laser frenectomy without any general anesthesia or sedation. After a quick in-office procedure, all five patients demonstrated increased lingual mobility evidenced by improved speech and feeding skills. Some improvements were observed immediately after the procedure by clinical staff and the child’s family. While these patients required continued intervention from a speech-language pathologist, their improved lingual mobility allowed for more significant and faster improvement in speech and feeding skills. These cases challenge the status quo that speech and feeding are not affected by posterior tongue-tie. Continued research is warranted to determine the impact that all classes of lingual restrictions can have on speech and feeding development.
Keywords: Ankyloglossia; Tongue-tie; Lip-tie; Frenum; Frenectomy; Speech issues; Feeding issues
| Introduction | ▴Top |
Infant feeding issues have been associated with tongue-ties in several studies in the last few decades [1-4]. These feeding issues include a poor or shallow latch, reflux and excessive spitting up, poor weight gain, gagging or choking, milk leakage, and frustration at the breast or with bottles [4-6]. Nipple pain, “lipstick”-shaped nipples, poor breast drainage, thrush, mastitis, and premature weaning are common for mothers with tongue-tied babies [4, 7]. Unfortunately, the diagnosis and treatment of tongue-tie is debated and misunderstood, leaving many infants with an undiagnosed tongue or lip-tie. While some lingual and labial restrictions are identified when the child is an infant or toddler, many health professionals only consider severe restrictions a concern (i.e. anterior tongue-tie). With other medical issues such as autism or sleep apnea, the medical community realizes that these conditions fit more onto a continuum or spectrum rather than a single disease state. Tongue-tie is not different. Ankyloglossia should be appreciated as a spectrum of restriction from the anterior to posterior sections of the tongue, as well as varying levels of elasticity and thickness. We are proposing a paradigm shift in the thinking of medical and dental professionals to encompass a wider scope of oral restrictions that cause difficulty with nursing, speech, and feeding.
Recently, the concept of posterior-tongue tie began gaining recognition in medical literature [4, 8-10]. Many infants demonstrate problems with nursing that don’t improve through traditional intervention. These babies do not present with a classic tether at the tip of the tongue, but often have a “posterior” or submucosal restriction due to a thick, tight, or short frenum. Releasing the posterior tongue-tie has demonstrated breastfeeding improvement for nursing babies [4, 7, 9], but there are currently no case reports or studies showing improvement with speech or solid feeding. As these children grow up, they may develop speech and feeding disorders that impact communication skills and quality of life. However, since there is no classic heart shape or “to-the-tip” tongue-tie, this puzzling presentation is difficult to diagnose. Often, even an anterior or classic tongue-tie is not considered a potential cause of disordered speech or feeding. The tongue is the primary organ concerned with these important skills, among a host of other functions. If an anatomical restriction, anterior or posterior, is causing a functional limitation, then understanding the impact of these restrictions on feeding and speech should be recognized by all medical, dental, and related health professionals who are evaluating and providing treatment for children.
In most cases, the children were referred to our office by speech-language pathologists or pediatricians for evaluation and treatment of their restricted frena. Information regarding speech, feeding, and oral health was gathered through the use of a questionnaire to assess whether functional limitations were present. By performing a full intraoral exam using the Kotlow classification for tongue-tie [11] and lip-tie [5, 12], paired with the concept of “functional ankyloglossia” from a recent article by Yoon et al [13], we were able to determine if the child had a restriction in tongue mobility that was likely causing an issue with feeding or speech. After obtaining informed consent from the parent, the release was performed in the dental office with no sedation or general anesthesia using a 10,600 nm LightScalpel CO2 laser (LS-1005, LightScalpel Inc. Bothell, WA) for all cases. Only local anesthesia was required. Post-operative stretches and exercises were recommended for 3 weeks, and a follow-up visit was scheduled 1 week after the procedure.
| Case Reports | ▴Top |
Case 1
A 5-year-old boy was referred to our office by his speech-language pathologist to assess candidacy for a tongue-tie release. He presented with disordered speech and feeding. Mom reported that he misarticulated the speech sounds /l/, /th/, /s/, /r/, and /m/. These speech sound errors were exacerbated as his rate of speech increased. Both familiar and unfamiliar listeners had difficulty understanding his speech. The patient also spoke softly and mumbled often. His mother described him as shy and lacking confidence in communication with others. He had received speech therapy for 2 months, where his therapist had targeted appropriate production of the /l/ sound. The patient also demonstrated selective eating and gagged on foods of various textures. Thick textures such as mashed potatoes were especially difficult for him to tolerate. His mother reported that he demonstrated difficulty in tolerating pureed foods as a baby. He had a strong gag reflex and also slept restlessly.
Upon examination, the patient was able to protrude his tongue past his lips and about one third of the way down his chin (Fig. 1a). He had relatively normal extension but was unable to elevate his tongue adequately to reach his palate when his mouth was fully open. He was diagnosed with a Kotlow Class II tongue-tie that is submucosal or posterior (Fig. 1b). He had a thick band of tissue for a frenum that was not easily observed unless the tongue was elevated, and thus was missed by other healthcare providers.
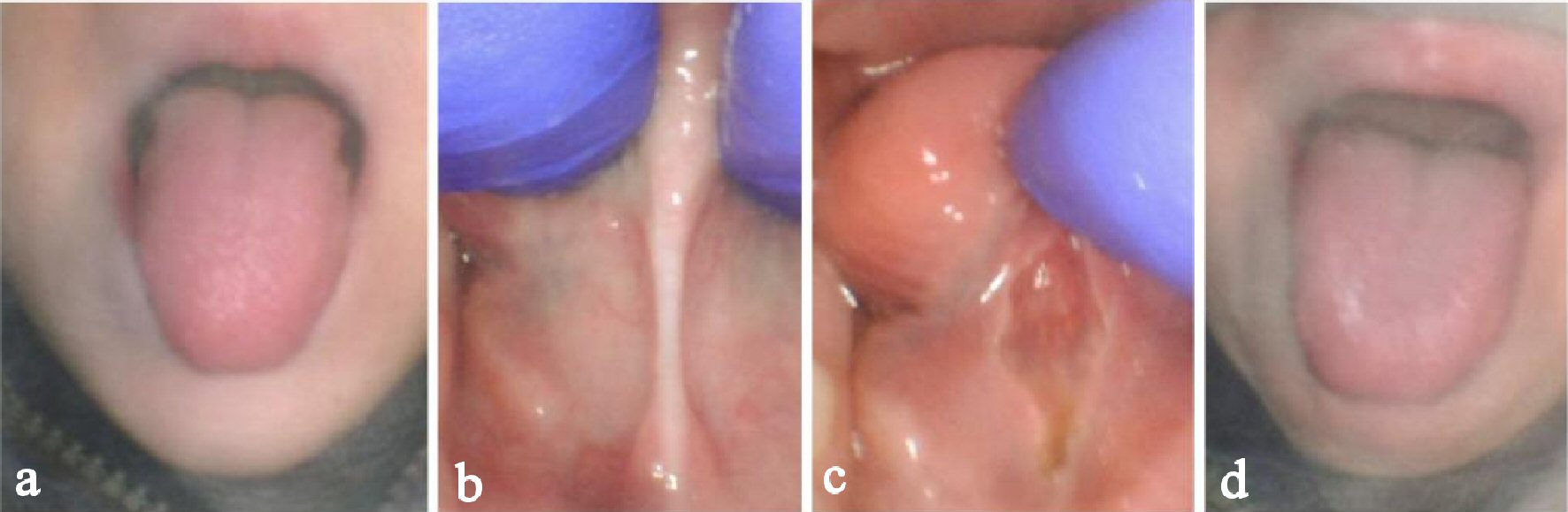 Click for large image | Figure 1. Case 1 of a 5-year-old male with hidden posterior tongue-tie. Before the procedure maximum protrusion (a) and digital elevation (b), immediately after the procedure maximum elevation (c) and maximum protrusion (d). |
The treatment was uneventful, and with nitrous oxide analgesia at 50% for 10 min, and 0.3 mL 2% lidocaine with 1:100,000 epi injected directly into the frenum, we were able to complete treatment without general anesthesia or sedation. We released all of the fibers in the frenum (mucosa and connective tissue) until the genioglossus muscle to provide normal range of motion and allow better elevation of the tongue (Fig. 1c). We used the CO2 laser pulsed at 29 Hz, Non-SuperPulse 2 W at 72.5% so an average power of 1.45 W. Immediate gains in tongue elevation and protrusion were noted by the doctor, patient, and parent (Fig. 1d). Follow-up exercises and stretching were recommended for 3 weeks.
Immediately after the procedure, his mother noticed improvement in speech intelligibility. At his follow-up visit 1 week later, his mother reported a continued improvement in speech intelligibility. Specifically, he was able to produce /s/ and /m/ with increased accuracy. She reported decreased gagging while eating. He had also tried new foods that mom said he would have never even attempted before. For example, he ate pork for dinner and quiche for breakfast. Prior to the frenectomy, he would have gagged or refused these food choices.
Case 2
This 5-year-old male was in foster care at time of the referral, so his birth and nursing history were unknown. The patient misarticulated the speech sounds /s/, /r/, and /ch/. He presented with a tongue thrust and jaw slide to the left when he talked or smiled. The patient demonstrated gagging and vomiting when eating a variety of textures, but primarily with soft foods. These behaviors had decreased since moving to his current foster home, but he continued to be averse to trying new foods. He frequently complained of neck pain.
The patient was diagnosed with a posterior tongue-tie (Kotlow class II). Due to the posterior nature of the tongue-tie, the tongue was elevated using digital pressure on either side of the restriction to confirm diagnosis (Fig. 2a). The child was given 50% nitrous oxide/50% oxygen for anxiolysis for 10 min and 0.3 mL 2% lidocaine with 1:100,000 epi was injected directly into the frenum. The CO2 laser was used for approximately 10 s beginning in the middle of the frenum. The laser was slowly moved from left to right in order to vaporize the frenum horizontally. The wound was approximately 2 mm deep with a diamond shaped appearance, which indicated a full release of tethered tissue including all mucosa and connective tissue (Fig. 2b). Follow-up exercises and stretching were recommended for 3 weeks.
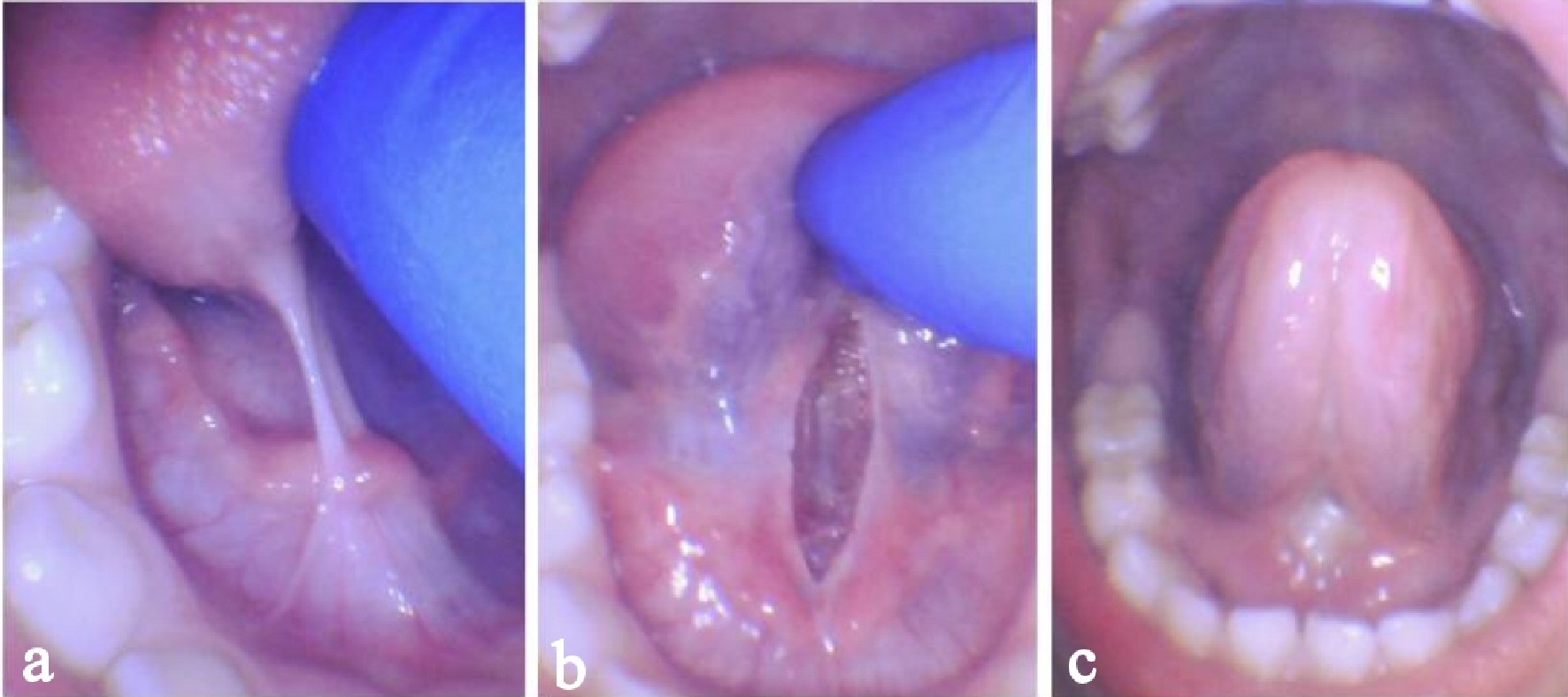 Click for large image | Figure 2. Case 2 of a 5-year-old male with posterior tongue-tie. Before the procedure maximum digital elevation (a), immediately after the procedure maximum digital elevation (b), healing at 1 week showing sustained elevation and increased mobility (c). |
At the 1 week follow-up, the patient reported no pain and demonstrated increased lingual elevation (Fig. 2c). His foster mother, a physical therapist, was very pleased with the child’s progress. She noted improved speech intelligibility, particularly with the speech sounds /s/, /r/, and /ch/. He demonstrated increased motivation in practicing new speech sounds. Range of motion in the neck was noted to be significantly improved by his foster mother, which was now allowing him to sleep comfortably on his stomach. She also indicated that the child took larger bites of food post-frenectomy. He ate foods including yogurt, potatoes, pudding, and cake without gagging or spitting out. These were food textures he would have previously not tolerated.
Case 3
This 11-year-old girl presented with disfluency and poor speech intelligibility (her mother reported “baby talk”, stuttering, and mumbling). She demonstrated particular difficulty with the speech sounds /th/ and /l/. The patient’s feeding history included poor nursing and latch, colic, and difficulty gaining weight. When the patient began eating solid foods, she demonstrated selective eating and a slow rate of intake. Her diet consisted of breads and sweets with minimal meat intake. The patient complained of neck pain daily (particularly in the morning) and demonstrated bruxism while sleeping. She demonstrated mouth breathing during the day and night and suffered from chronic sinus infections.
The patient presented with a narrow palate with a high arch. She was diagnosed with a posterior tongue-tie (Kotlow Class II). Due to the posterior nature of the tongue-tie, the tongue was elevated using digital pressure on either side of the restriction to confirm diagnosis (Fig. 3a). Minimal lingual protrusion past the lips was observed, and lingual elevation was limited (Fig. 3b). She successfully elevated her tongue to approximately 50% of her maximal mouth opening.
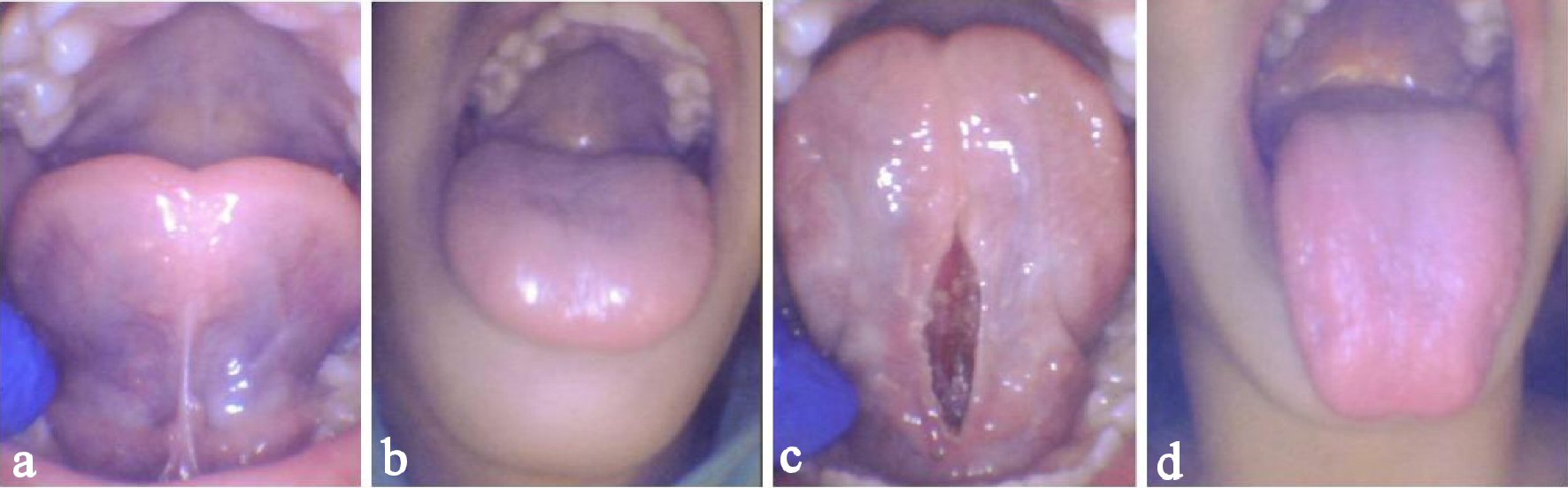 Click for large image | Figure 3. Case 3 of an 11-year-old female with posterior tongue-tie and impaired elevation and protrusion. Before the procedure maximum elevation (a) and protrusion (b), immediately after the procedure maximum elevation (c) and protrusion (d). |
The patient was given nitrous oxide for anxiolysis and 0.3 mL 2% lidocaine 1:100,000 epi was injected into the frenum. The tissue was vaporized with the CO2 laser at an average power of 1.45 W for approximately 20 s. The patient was observed to tolerate the procedure well and noted feeling no pain. Elevation and protrusion were significantly improved immediately (Fig. 3c, d). Follow-up exercises and stretching were recommended for 3 weeks. Her mother reported improved speech intelligibility immediately after the procedure and noted the presence of speech sounds that the patient was previously unable to produce. The patient noted immediate relief from neck tension. During a follow-up phone call 3 weeks later, the patient’s mother noted marked improvement in speech intelligibility and more appropriate food intake. She was consistently eating “full meals”. The patient and her mother reported an improved quality of sleep and significantly decreased neck tension.
Case 4
This is a 2 years and 10 months old boy who was referred by his speech-language pathologist for assessment of candidacy for a tongue-tie release. The patient did not begin babbling until 2 years of age and currently says approximately 30 words. He has received speech therapy for 1 year and has made minimal progress. His speech was difficult for both familiar and unfamiliar listeners to understand. The patient demonstrates food packing in both cheeks at times, but demonstrated no other feeding concerns. He has a history of chronic ear infections.
Upon examination, he was diagnosed with a posterior Kotlow Class I tongue-tie that was only visible with retraction (Fig. 4a). Although the area appeared normal at first glance, the tissue was tight and demonstrated minimal elasticity when manipulated. Prior to the frenectomy, the tongue was anesthetized with topical numbing jelly of 2.5% lidocaine, 2.5% prilocaine. The CO2 laser was used at 1.45 avg. W for 5 s. The patient demonstrated discomfort during the procedure, but calmed immediately once completed. Tongue elevation was immediately improved, and the sublingual area felt soft and spongy with normal elasticity (Fig. 4b). Follow-up exercises and stretching were recommended for 3 weeks.
 Click for large image | Figure 4. A 2-year-old male with hidden posterior tongue-tie. Before the release maximum elevation (a), immediately after the release elevation demonstrating no bleeding and diamond shaped wound with increased elevation (b). |
At the patient’s 1 week follow-up, his mother reported significant improvement. He is now babbling most of the day, and he began verbalizing more variety of vowels and early developing consonant sounds. Soon after the procedure, the patient began using new words (i.e. “ice”) and combining words into short phrases (i.e. “up me”). He appeared to communicate wants and needs more effectively and began imitating non-speech sounds (i.e. animal sounds). His mother reported that he is less frustrated and generally happier. Although feeding wasn’t much of a concern prior to the procedure, the patient’s mother reports a noticeable difference in rate and amount of intake (“He is eating a lot more and much faster”), and he stopped food packing.
Case 5
This 17-month-old girl presented with a speech and language delay. She began babbling at 15 months and said only a few words, including “mama” and “dada” at time of the assessment. Her pediatrician and gastroenterologist recommended an upper GI scope and a modified barium swallow due to a history of digestive and swallowing issues, including frequent choking on liquids. As an infant, the patient demonstrated poor latch when breastfeeding and bottle feeding, poor weight gain, reflux, and colic. The mother experienced painful nursing. Mom also communicated that it was difficult to brush the patient’s maxillary anterior teeth. The patient woke frequently during the night and demonstrated restlessness while sleeping.
Upon intraoral examination, the patient was diagnosed with a significant maxillary lip-tie (Kotlow Class IV) and a posterior tongue-tie (Kotlow Class II). Blanching of the maxillary frenum was evident upon retraction and presence of a diastema was observed (Fig. 5a). The posterior tongue-tie was visible and easily palpated by running a finger across the floor of the mouth (Fig. 5b). The lingual frenum felt like a tight string with minimal elasticity. A topical numbing jelly consisting of 2.5% lidocaine/2.5% prilocaine was applied inside the upper lip and under the tongue. A few drops of 2% lidocaine with 1:100:000 epi was injected into the maxillary frenum. No sedation, nitrous, or general anesthesia was required. The CO2 laser procedure lasted approximately 15 s for the maxillary frenum release at an average of 2.1 W, and 5 s for the lingual frenum release at an average of 1.45 W. Immediately greater mobility was noticed with the maxillary lip, and greater elevation was noted with the tongue (Fig. 5c, d). No stitches were required, and follow-up exercises and stretching were recommended for 3 weeks.
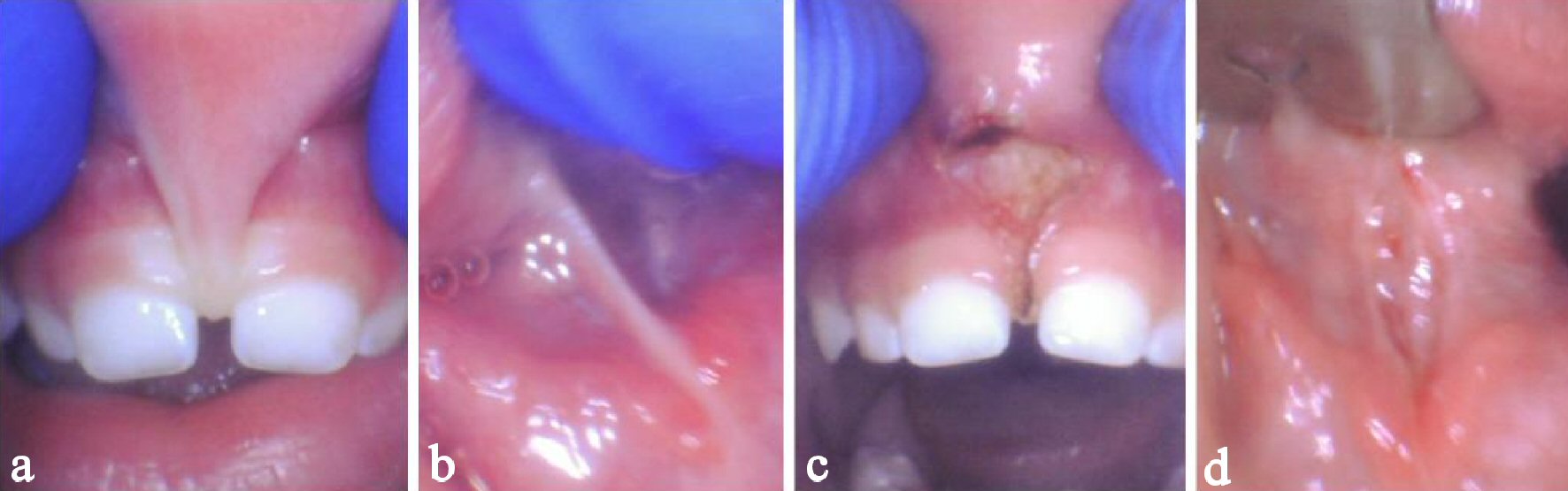 Click for large image | Figure 5. One 17-month-old girl with restrictive maxillary lip-tie and posterior tongue-tie. Before the release lip-tie (a) and posterior tongue-tie (b). Immediately after the release increased maxillary lip elevation (c) and tongue elevation (d). |
Her mother reported that the first day, immediately after the procedure, she said four new words: bubba, pawpaw, juice, and hot. She also reported that the patient did not choke on liquids or spit up since the procedure. Her mother reported that the quality of her voice improved (“her voice is louder, clearer, and not as raspy”).
| Discussion | ▴Top |
Three procedures are often used to release tethered oral tissue: frenotomy, frenectomy and frenuloplasty. A frenotomy is a “snip” or “clip” of the frenum and often leaves a thick posterior area of the frenum untouched. It offers some improvement in length or mobility, and when multiple cuts are made, a full release is possible, but often one cut with scissors leaves an incomplete release. A frenectomy involves removal of the frenum by excising the tissue using a laser, scalpel, or scissors. Frenuloplasty aims to lengthen the tongue by performing specific incision and wound closure methods involving sutures and can be completed using a laser, scalpel, or scissors. All of the cases reported above were frenectomies using a CO2 laser, which are reported to cause less post-procedure pain than release procedures using scalpels [14]. Use of a laser also allows for excellent hemostasis and surgical control, as well as remarkable wound healing without sutures required [14]. Dental lasers, particularly the CO2 laser, have revolutionized the frenectomy procedure. It can now be performed as a minor, in office procedure without the need for general anesthesia or sedation. Frenectomies or frenuloplasties performed using traditional methods such as a scalpel or scissors often require sedation or general anesthesia [15]. Researchers are not convinced that the use of anesthesia in children is safe, particularly for infants and children under age 2 [16, 17].
Release procedures using lasers only require local anesthetic in the form of a topical gel or injection to the surgical area. Frenectomies performed by laser are often completed in a matter of seconds, while surgeries that require sedation or general anesthesia require a longer time commitment, higher cost, and greater risk. Intraoperative surgical risks with laser are exceedingly rare. Since a laser is inherently bactericidal, this method of release is especially low risk for infection [18]. Post-operative infection has never been documented. Minimal to moderate bleeding is possible, but is easily managed with gauze and pressure. In fact, most laser wounds have no bleeding at all. An experienced clinician will minimize the bleeding risk by keeping the diamond wound narrow to avoid exposing the superficial veins under the tongue.
Laser safety protocols were followed strictly during all procedures, including eye protection for everyone in the room (including the patient) in all cases referenced in this article. Each procedure was performed using a 10,600nm CO2 laser (LS-1005, LightScalpel Inc., Bothell, WA). The laser settings vary based on tissue type, but the patients generally received 2 W pulsed at 72.5% duty cycle and 29 Hz so 1.45 W average power for 10 - 20 s. Before and after pictures of each restriction are critical to documentation, family education, and protection in case of an audit. We take before and after videos or speech samples to informally assess differences in speech intelligibility. As stated above, there’s often an immediate difference as observed by the parent, patient, clinician, and other caregivers. Typical results include a clearer and louder voice, as well as immediate improvement in affected speech sounds.
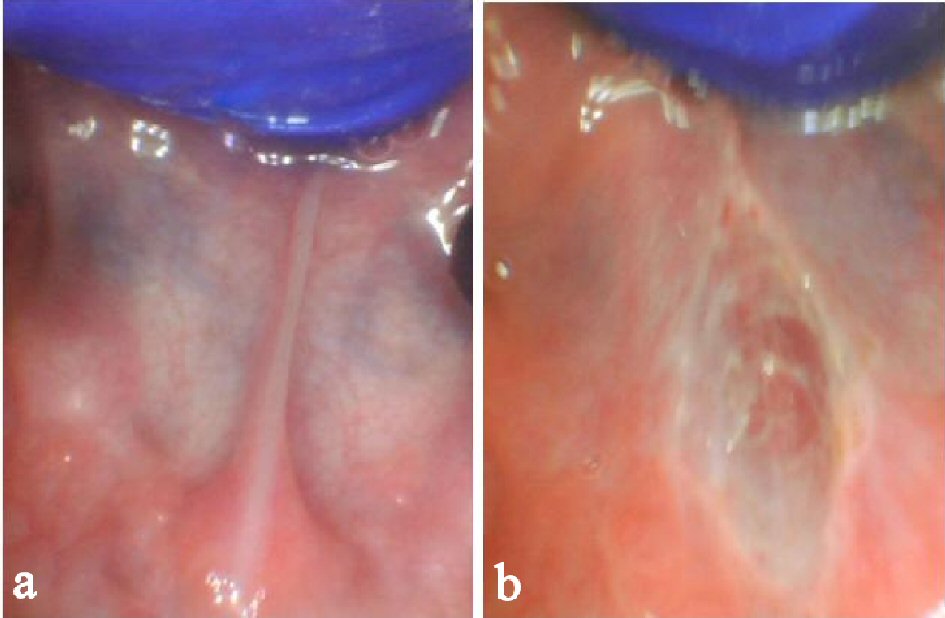
We have encountered patients who demonstrate limited progress in functional oral skills (i.e. chewing, speech intelligibility) post-frenotomy performed using a scalpel or scissors due to a partial release. In our clinical experience, frenectomies performed by laser more consistently result in a complete release of the tethered oral tissue due to increased visibility and surgical precision. Some patients (none in this series) originally present with a posterior tongue-tie created after an incomplete frenotomy or ineffective stretching protocol. For example, the infant represented in Figure 6a continued to demonstrate difficulties in breastfeeding post-frenotomy using scissors. After releasing the posterior aspect of the frenum properly with the CO2 laser, the symptoms disappeared (Fig. 6b). Incomplete release procedures may account for the inconsistent results seen from frenotomy/frenectomies in the past [19]. Many patients who saw minimal improvement in speech or feeding post-frenotomy may have received an incomplete release or suffered from ineffective wound management, causing the frenum to reattach.
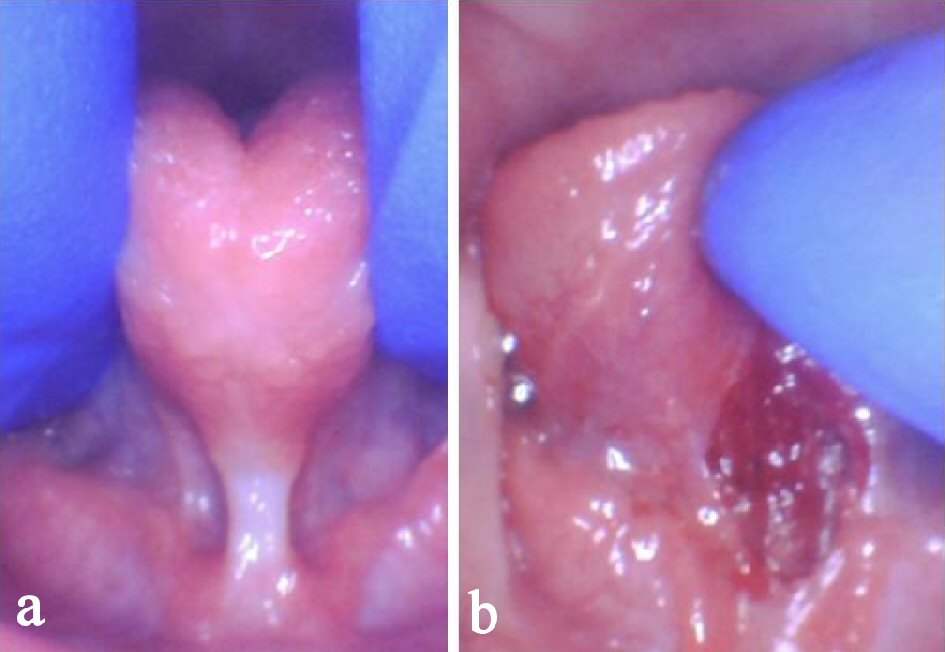 Click for large image | Figure 6. Improperly released tongue after scissors frenotomy showing impaired tongue elevation and thick band of fibrous tissue (a). Immediately after the release showing diamond-shaped wound, hemostasis, and increased elevation of tongue (b). |
Wound management is a vital step in the frenectomy process, especially when sutures are not used because the area heals by secondary intention instead of primary closure. If proper wound management is not performed, a process known as reattachment can occur allowing the area to heal back together and decrease mobility, thus limiting function. A wound management protocol involving stretches and strengthening exercises ensure that the tissue remains free from restriction as the wound heals. We recommended the parents to perform active wound management stretches three times a day for 3 weeks using gentle but firm pressure to lift the tongue and the lip to keep the wound separated. This stretch put tension on the wound to ensure it did not grow back together. Visualization of the diamond during stretches with a flashlight was encouraged to ensure the diamond wound healed as much as possible in an elongated position. Further, myofunctional tongue exercises to strengthen the tongue in various positions (elevation, protrusion, lateral extension, and clicking noises) were encouraged. A 1 week follow-up visit is integral to success and if needed, a deeper stretch can be performed by the provider if the area shows signs of restriction or reattachment. Reattachment poses the most significant risk to the success of the release procedure.
Speech and feeding deficits that result from the presence of tethered oral tissues are not likely to be corrected through traditional speech therapy alone. Inefficient structure will limit progress and must be corrected for the patient to receive the full benefit of speech and feeding intervention. Frenectomy is a low risk, in office procedure that can allow for functional improvement in speech intelligibility, sound acquisition, and feeding success. As seen in the case studies discussed above, the results are variable and never guaranteed. However, most patients who receive a frenectomy demonstrate some progress in the development of appropriate feeding skills, improved speech intelligibility, or increased speech sound acquisition. Historically, articulation errors decrease after tongue-tie release [20-22].
The existence of submucosal/posterior tongue-ties continues to be debated among health professionals. They are often identified through reported or observed symptoms, as they are sometimes difficult to detect through visual or physical assessment. Unfortunately, many individuals with a posterior tongue-tie go years before the restriction is identified. It’s interesting that individuals who suffer from tethered oral tissues consistently present with seemingly unrelated symptoms such as neck pain and tension, poor sleep quality, headaches, and bruxism. In our experience and others, these symptoms, along with functional deficits in speech and feeding skills, often improve after a successful release procedure, regardless of whether an anterior or posterior tongue-tie is present.
Tethered oral tissue assessment and treatment require a team approach involving a speech-language pathologist, myofunctional therapist, pediatrician, and release provider. Release of a restricted frenum provides a patient the opportunity for adequate lingual range of motion, but evaluation by a speech-language pathologist or oral function specialist is required to determine whether function is adequate for speech, feeding, and oral health. Many patients who present with tethered oral tissue develop compensatory strategies and poor oral habits that require treatment to ensure the improvement of oral function [19]. Assessment and therapy by a speech-language pathologist or oral function specialist is necessary to ensure the patient receives the full benefit from the release procedure.
At this time, literature to support structural correction followed by speech and/or feeding intervention is lacking. We plan on initiating a prospective trial in the near future to quantify the progress we are seeing with this method. Current data support a positive relationship between a successful frenectomy and improvement in speech and feeding skills, but continued quality research is warranted to support the apparent benefits of release procedures.
Consent
Written informed consent was obtained from the parents for all of these procedures.
Conflict of Interest
The authors declare no conflict of interest.
| References | ▴Top |
- Berry J, Griffiths M, Westcott C. A double-blind, randomized, controlled trial of tongue-tie division and its immediate effect on breastfeeding. Breastfeed Med. 2012;7(3):189-193.
doi pubmed - Buryk M, Bloom D, Shope T. Efficacy of neonatal release of ankyloglossia: a randomized trial. Pediatrics. 2011;128(2):280-288.
doi pubmed - Emond A, Ingram J, Johnson D, Blair P, Whitelaw A, Copeland M, Sutcliffe A. Randomised controlled trial of early frenotomy in breastfed infants with mild-moderate tongue-tie. Arch Dis Child Fetal Neonatal Ed. 2014;99(3):F189-195.
doi pubmed - Ghaheri BA, Cole M, Fausel SC, Chuop M, Mace JC. Breastfeeding improvement following tongue-tie and lip-tie release: A prospective cohort study. Laryngoscope. 2017;127(5):1217-1223.
doi pubmed - Kotlow LA. Oral diagnosis of abnormal frenum attachments in neonates and infants: evaluation and treatment of the maxillary and lingual frenum using the Erbium: YAG laser. J Pediatric Dent Care. 2004;10:11-14.
- Siegel SA. Aerophagia induced reflux in breastfeeding infants with ankyloglossia and shortened maxillary labial frenula (Tongue and Lip Tie). International Journal of Clinical Pediatrics. 2016;5:6-8.
doi - Kotlow L. Diagnosis and treatment of ankyloglossia and tied maxillary fraenum in infants using Er:YAG and 1064 diode lasers. Eur Arch Paediatr Dent. 2011;12(2):106-112.
doi pubmed - Crenshaw JT. Healthy birth practice #6: keep mother and baby together- it's best for mother, baby, and breastfeeding. J Perinat Educ. 2014;23(4):211-217.
doi pubmed - Coryllos E, Genna CW, Salloum AC, et al. Congenital tongue-tie and its impact on breastfeeding. Breastfeeding: Best for Mother and Baby. American Academy of Pediatrics; 2004;1-6.
- Chu MW, Bloom DC. Posterior ankyloglossia: a case report. Int J Pediatr Otorhinolaryngol. 2009;73(6):881-883.
doi pubmed - Kotlow LA. Ankyloglossia (tongue-tie): a diagnostic and treatment quandary. Quintessence Int. 1999;30(4):259-262.
pubmed - Kotlow LA. Diagnosing and understanding the maxillary lip-tie (superior labial, the maxillary labial frenum) as it relates to breastfeeding. J Hum Lact. 2013;29(4):458-464.
doi pubmed - Yoon A, Zaghi S, Weitzman R, Ha S, Law CS, Guilleminault C, Liu SYC. Toward a functional definition of ankyloglossia: validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 2017;21(3):767-775.
doi pubmed - Haytac MC, Ozcelik O. Evaluation of patient perceptions after frenectomy operations: a comparison of carbon dioxide laser and scalpel techniques. J Periodontol. 2006;77(11):1815-1819.
doi pubmed - Kupietzky A, Botzer E. Ankyloglossia in the infant and young child: clinical suggestions for diagnosis and management. Pediatr Dent. 2005;27(1):40-46.
pubmed - Reddy SV. Effect of general anesthetics on the developing brain. J Anaesthesiol Clin Pharmacol. 2012;28(1):6-10.
doi pubmed - Mellon RD, Simone AF, Rappaport BA. Use of anesthetic agents in neonates and young children. Anesth Analg. 2007;104(3):509-520.
doi pubmed - Kato T, Kusakari H, Hoshino E. Bactericidal efficacy of carbon dioxide laser against bacteria-contaminated titanium implant and subsequent cellular adhesion to irradiated area. Lasers Surg Med. 1998;23(5):299-309.
doi - Fernando C. Tongue tie - from confusion to clarity: a guide to the diagnosis and treatment of ankyloglossia. Tandem Publications. 1998.
- Messner AH, Lalakea ML. The effect of ankyloglossia on speech in children. Otolaryngol Head Neck Surg. 2002;127(6):539-545.
doi pubmed - Lalakea ML, Messner AH. Ankyloglossia: the adolescent and adult perspective. Otolaryngol Head Neck Surg. 2003;128(5):746-752.
doi - Ito Y, Shimizu T, Nakamura T, Takatama C. Effectiveness of tongue-tie division for speech disorder in children. Pediatr Int. 2015;57(2):222-226.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
