| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website https://www.theijcp.org |
Case Report
Volume 12, Number 1, May 2023, pages 11-14
Methylene Blue Infiltration During Intraoperative Anesthetic Care
Sidhant Kalsotraa, Katherine Stakera, Renee Henga, b, Joseph D. Tobiasa, b, c
aDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
bDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
cCorresponding Author: Joseph D. Tobias, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA
Manuscript submitted November 14, 2022, accepted November 28, 2022, published online March 28, 2023
Short title: Methylene Blue Infiltration
doi: https://doi.org/10.14740/ijcp504
| Abstract | ▴Top |
Following its initial synthesis in 1876, methylene blue has been used in various clinical scenarios for diagnostic and treatment purposes. In general, its adverse effect profile is relatively limited. We present a 22-year-old patient who experienced extravasation of methylene blue intended for intravenous administration during cystoscopy with retrograde pyelogram. The clinical uses of methylene blue are reviewed, risks and adverse effects associated with its administration discussed, and options reviewed for the treatment of inadvertent extravasation.
Keywords: Methylene blue; Pediatric anesthesiology; Infiltration
| Introduction | ▴Top |
Methylene blue (methylthioninium chloride) is an organic chloride salt. It was originally synthesized in 1876 as an aniline-based dye for the textile industry. However, it was subsequently identified as an agent that had potential for use in microscopy staining [1]. Observations of its selective staining and inactivation of microbial species led to the testing of aniline-based dyes as a topical antiseptic agent and for the treatment of tropical diseases including malaria. Subsequently, it has been used clinically for a variety of indications including sentinel lymph node tracing, reversal of methemoglobinemia, and the treatment of postoperative vasoplegia and distributive shock [2-4]. Despite a long history of use in various clinical scenarios, the reported adverse effect profile of methylene blue remains limited. We present a 22-year-old patient who experienced extravasation of methylene blue intended for intravenous (IV) administration during cystoscopy with retrograde pyelogram. The clinical uses of methylene blue are reviewed, risks and adverse effects associated with its administration discussed, and options reviewed for the treatment of inadvertent extravasation.
| Case Report | ▴Top |
Review of this case and presentation in this format followed the guidelines of the Institutional Review Board of Nationwide Children’s Hospital (Columbus, Ohio). The patient was a 22-year-old male who presented for treatment of nephrolithiasis. The patient had a complex past medical history significant for myelomeningocele (MMC), solitary left kidney, chronic kidney disease, neurogenic bowel and bladder, recurrent urinary tract infections, hydrocephalus with ventriculo-peritoneal shunt placement, and an indwelling suprapubic catheter after prior bladder reconstruction. He presented with an acute deterioration of renal function with concern for genito-urinary tract obstruction due to nephrolithiasis. Radiological imaging suggested distal ureteral obstruction with dilation of the ureter in his solitary left ureter, necessitating urgent cystoscopy with retrograde left ureteral stent placement. Preoperative vital signs included a blood pressure of 142/74 mm Hg, pulse of 126 beats/min, respirations of 20 breaths/min, oxygen saturation of 97%, and a temperature of 37.1 °C (98.7 °F). Physical examination including cardiac, respiratory, and neurological evaluations was unremarkable. Preoperative and postoperative laboratory values are shown in Table 1. He was transported to the operating room and routine American Society of Anesthesiologists’ monitors were placed. Given the urgent nature of the procedure, his inadequate nil per os time, and the presence of lack of sensation to the perineum and lower extremities due to the MMC, the patient consented to proceed with procedural sedation in an attempt to avoid general anesthesia. Sedation was provided with IV midazolam (total of 4 mg administered in two doses) and IV fentanyl (total dose of 75 µg). Cystoscopy proceeded without difficulty; however, the left ureteral orifice could not be identified. Visualization was difficult due to bladder trabeculations, chronic bladder inflammation, and the prior ureteral reimplantation procedure. To provide visualization of the ureteral orifice, methylene blue (ProvayBlue® 5 mg/mL) was administered intravenously (initial dose of 5 mL or 25 mg IV). During administration, the patient complained of burning at the injection site; however, no infiltration or local concerns were noted at the injection site. The IV infusion continued to drip freely by gravity and systemic administration of methylene blue was confirmed by a spurious decrease in the oxygen saturation as measured by pulse oximetry. As the desired effect was not achieved with the first dose of methylene blue, second and third doses (12.5 mg or 2.5 mL IV) were administered for a total intraoperative dose of 50 mg IV. After approximately 1 h of attempting to identify the ureteral orifice, the decision was made to stop the procedure. Upon removal of the surgical drapes, the peripheral IV site was noted to be infiltrated. The left forearm was swollen and indurated. The peripheral IV was removed and a cannula was placed in the other arm. The affected arm and hand had a capillary refill of less than 3 s with intact pulses. There was painful swelling with greenish-blue discoloration from the methylene blue infiltration in the area surrounding the previous IV cannula (Fig. 1). The vascular access team was consulted to provide treatment recommendations. Treatment options were further discussed with the pharmacy as methylene blue infiltration is encountered with extreme infrequency at our institution. The decision was made to locally infiltrate the subcutaneous tissues with hyaluronidase followed by the placement of topical nitroglycerin paste. The remainder of the postoperative course was unremarkable. There was gradual resolution of the tissue swelling and discoloration of the left forearm over the ensuring 48 h with no signs of tissue necrosis. There was a gradual decrease in the creatinine and blood urea nitrogen (BUN) back to baseline values of 1.5 - 1.8 and 25 - 35 mg/dL. The cause of the acute deterioration of renal function was determined to be urosepsis with acute on chronic renal insufficiency. The patient was discharged home without evidence of tissue or skin necrosis. Follow-up 3 months later reveals no residual damage to the forearm.
 Click to view | Table 1. Preoperative and Postoperative Laboratory Values |
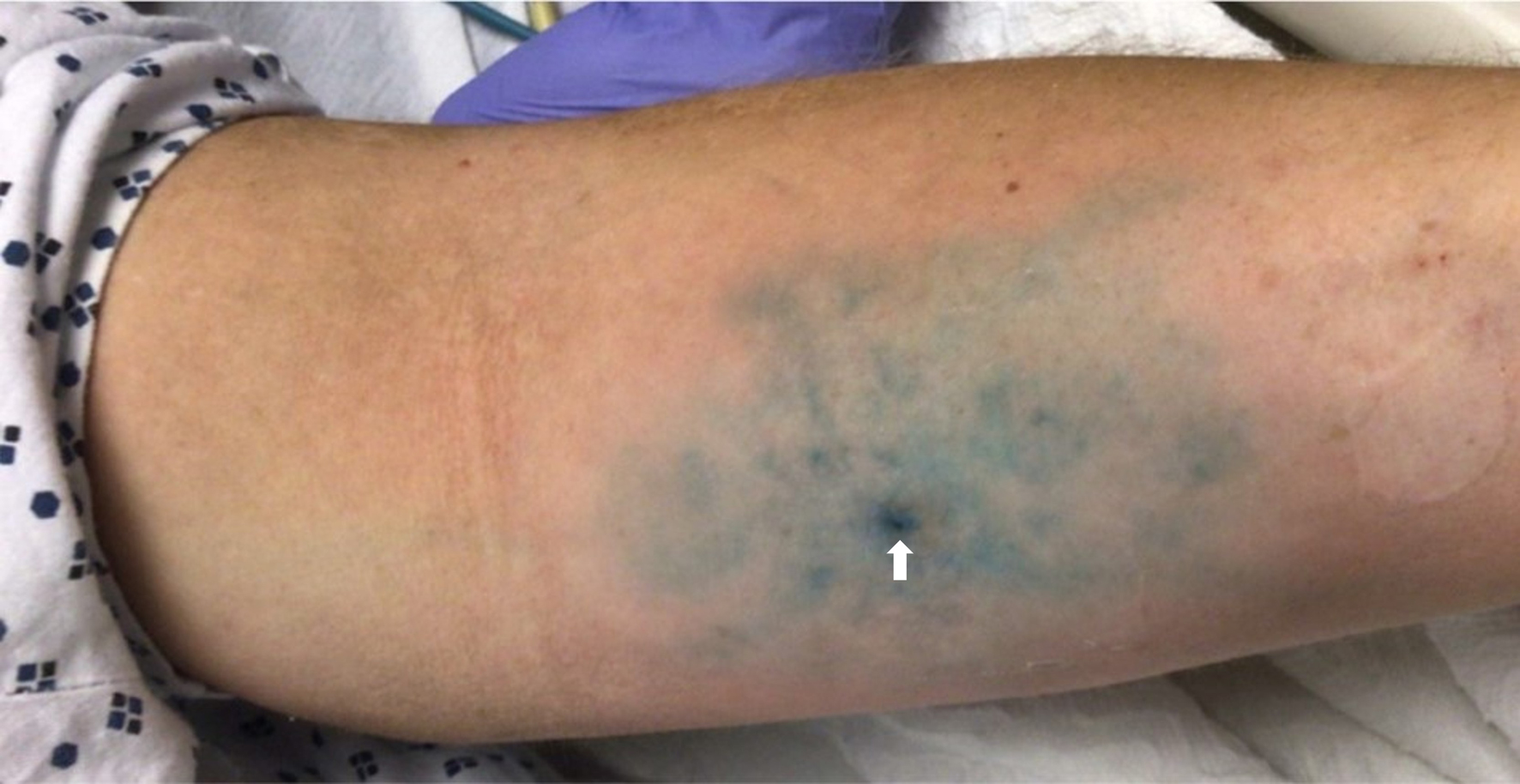 Click for large image | Figure 1. Swelling around the intravenous cannula site on the left forearm with green/blue discoloration from the methylene blue extravasation in the area surrounding the site of the previous intravenous cannula (white arrow). |
| Discussion | ▴Top |
The described case report outlines a unique and potentially unrecognized complication of methylene blue administration, tissue necrosis with inadvertent extravasation during IV administration. Previously reported cases have focused on complications of intentional administration of methylene blue for sentinel lymph node tracing in breast cancer patients or on extravasation occurring in the setting of continuous infusion of methylene blue. Here we have presented a case of inadvertent extravasation during bolus administration. Despite a high therapeutic index with a limited adverse effect profile, the literature contains anecdotal evidence to suggest that significant tissue necrosis can occur with extravasation of methylene blue. As such, close attention to the IV access site is recommended during administration. Even with such precautions, extravasation can occur as was noted in our patient. When significant extravasation occurs, therapeutic interventions may be indicated to prevent loss of limb.
The adverse effect profile of methylene blue is limited and consists of mild, non-generalized systemic signs and symptoms such as headache, nausea, vomiting, confusion, shortness of breath, and high blood pressure [5]. More serious albeit uncommon adverse effects include allergic reactions, hemolysis, and serotonin syndrome through inhibition of monoamine oxidase [6, 7]. Blue-green discoloration of the urine, sweat, and stool also occur. Additionally, administration results in an abrupt and spurious decrease in the pulse oximeter reading [8].
There have also been rare reports of local effects including erythema, ulceration, and tissue necrosis with inadvertent extravasation during IV administration or subcutaneous and intradermal injection for lymphatic mapping during oncological surgery [9-13]. Various mechanisms have been proposed to explain the local tissue effects of methylene blue. As it inhibits the nitric oxide-mediated cGMP pathway, local vasoconstriction of arterioles may occur resulting in tissue ischemia. Additionally, methylene blue may have direct cytotoxic effects from the chemical itself, the low pH (3-4.5) or high osmolarity of the solution, or metabolism to formaldehyde and deaminized oxide radicals. These toxic tissue effects have been described regardless of the route of administration and the clinical indication for methylene blue. The degree and the severity of the tissue necrosis are likely related to the concentration and volume of the extravasated methylene blue [14]. As was used in the patient, it is recommended to use a 0.5% solution with slow incremental administration.
When extravasation of irritant solutions occurs, treatment depends on the solution that is infiltrated and the impact on the extremity. The IV infusion should be stopped immediately to prevent ongoing infiltration and any residual medication aspirated from the administration site. Constricting bands or tape should be removed from the involved extremity. The extremity should be elevated and distal perfusion assessed. In our patient, although infiltration and swelling were noted, there was no vascular compromise as capillary refill and pulses were intact. In cases with full-thickness skin necrosis compromising perfusion, manifesting as loss of peripheral pulses, or poor capillary refill, fasciotomy may be required [15, 16]. For less extensive infiltrations, local management is generally acceptable. The use of specific antidotes such as phentolamine for vasoconstrictor agents (dopamine or norepinephrine) or non-specific agents such as hyaluronidase or topical nitroglycerin may help restore perfusion. Hyaluronidase is postulated to break down hyaluronic acid, dispersing tissue planes thereby allowing for spread and dilution of the medication [17, 18]. Nitroglycerin forms nitric oxide free radicals, which activate guanylate cyclase increasing cGMP resulting in a local vasodilatory effect on peripheral veins and arterioles, diminishing the vasoconstrictive effects of methylene blue. Anecdotal experience has also proposed the use of liposuction to remove the medication from the subcutaneous tissues [13].
In conclusion, despite its relative safety in clinical practice, the extravasation of methylene blue during IV administration can result in local tissue reaction, ischemia, and necrosis. Although administration through a central venous catheter has been recommended, such a practice is not universally feasible. IV administration should occur only through a properly functioning and freely flowing peripheral IV catheter. The site should be monitored regularly during and after administration. The administration should stop promptly if there is pain on injection or concerns of extravasation.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Consent was obtained from the patient for anesthetic care and the use of deidentified information for teaching or publication.
Author Contributions
SK: case review and preparation of manuscript; KS and RH provided intraoperative care of the patient and review of the final manuscript; JDT: manuscript preparation, review, and editing.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Oz M, Lorke DE, Hasan M, Petroianu GA. Cellular and molecular actions of Methylene Blue in the nervous system. Med Res Rev. 2011;31(1):93-117.
doi pubmed - Kwok ES, Howes D. Use of methylene blue in sepsis: a systematic review. J Intensive Care Med. 2006;21(6):359-363.
doi pubmed - Marczin N, Tekeres M, Salzman AL, Szabo C. Methylene blue infusion in septic shock. Crit Care Med. 1995;23(11):1936-1938.
doi pubmed - Schirmer RH, Coulibaly B, Stich A, Scheiwein M, Merkle H, Eubel J, Becker K, et al. Methylene blue as an antimalarial agent. Redox Rep. 2003;8(5):272-275.
doi pubmed - Clifton J, 2nd, Leikin JB. Methylene blue. Am J Ther. 2003;10(4):289-291.
doi pubmed - Dewachter P, Castro S, Nicaise-Roland P, Chollet-Martin S, Le Beller C, Lillo-le-Louet A, Mouton-Faivre C. Anaphylactic reaction after methylene blue-treated plasma transfusion. Br J Anaesth. 2011;106(5):687-689.
doi pubmed - Gillman PK. Methylene blue implicated in potentially fatal serotonin toxicity. Anaesthesia. 2006;61(10):1013-1014.
doi pubmed - Rong LQ, Mauer E, Mustapich TL, White RS, Di Franco A, Girardi LN, Gaudino M, et al. Characterization of the rapid drop in pulse oximetry reading after intraoperative administration of methylene blue in open thoracoabdominal aortic repairs. Anesth Analg. 2019;129(5):e142-e145.
doi pubmed - Perry PM, Meinhard E. Nectotic subcutaneous abscesses following injections of methylene blue. Br J Clin Pract. 1974;28(8):289-291.
- Stradling B, Aranha G, Gabram S. Adverse skin lesions after methylene blue injections for sentinel lymph node localization. Am J Surg. 2002;184(4):350-352.
doi pubmed - Dumbarton TC, Gorman SK, Minor S, Loubani O, White F, Green R. Local cutaneous necrosis secondary to a prolonged peripheral infusion of methylene blue in vasodilatory shock. Ann Pharmacother. 2012;46(3):e6.
doi pubmed - Aydogan F, Celik V, Uras C, Salihoglu Z, Topuz U. A comparison of the adverse reactions associated with isosulfan blue versus methylene blue dye in sentinel lymph node biopsy for breast cancer. Am J Surg. 2008;195(2):277-278.
doi pubmed - Khokhar RS, Aqil M, Al-Zahrani T, Gelidan A, Al Khayal K. Novel management of methylene blue extravasation: A case report and review of literature. Saudi J Anaesth. 2015;9(2):211-213.
doi pubmed - Thevarajah S, Huston TL, Simmons RM. A comparison of the adverse reactions associated with isosulfan blue versus methylene blue dye in sentinel lymph node biopsy for breast cancer. Am J Surg. 2005;189(2):236-239.
doi pubmed - Shenaq SM, Abbase EH, Friedman JD. Soft-tissue reconstruction following extravasation of chemotherapeutic agents. Surg Oncol Clin N Am. 1996;5(4):825-845.
doi pubmed - Scuderi N, Onesti MG. Antitumor agents: extravasation, management, and surgical treatment. Ann Plast Surg. 1994;32(1):39-44.
doi pubmed - Reynolds PM, MacLaren R, Mueller SW, Fish DN, Kiser TH. Management of extravasation injuries: a focused evaluation of noncytotoxic medications. Pharmacotherapy. 2014;34(6):617-632.
doi pubmed - Zucker G. Use of phentolamine to prevent necrosis due to levarterenol. J Am Med Assoc. 1957;163(16):1477-1479.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
