| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website http://www.theijcp.org |
Case Report
Volume 7, Number 3, September 2018, pages 36-38
Non-Infectious Parotitis in Infants with Severe Bronchopulmonary Dysplasia: A Case Series
Jotishna Sharmaa, b, c, Charisse Lachicaa, b, Winston Manimtima, b
aDepartment of Pediatrics, Children’s Mercy-Kansas City, Kansas City, MO, USA
bUniversity of Missouri-Kansas City School of Medicine, Kansas City, MO, USA
cCorresponding Author: Jotishna Sharma, Department of Pediatrics, Children’s Mercy-Kansas City, 2401 Gillham Road, Kansas City, MO 64108, USA
Manuscript submitted May 14, 2018, accepted June 13, 2018
Short title: Non-Infectious Parotitis in Infants
doi: https://doi.org/10.14740/ijcp302w
| Abstract | ▴Top |
We report four former extremely premature infants with severe bronchopulmonary dysplasia (BPD) who had tracheostomy for prolonged mechanical ventilation and presented with non-infectious parotitis while still in the neonatal intensive care unit. A retrospective chart review of patients with BPD who developed parotitis was conducted over a 5-year period at a level IV neonatal intensive care unit with a BPD home ventilator program. During this 5-year period, there were 409 patients with BPD, and 48 (11.7%) of these patients had a tracheostomy (severe BPD). Four patients with severe BPD with tracheostomy and on mechanical ventilation developed non-infectious parotitis. All four patients initially underwent an infectious work-up, which were negative. Non-infectious parotitis can complicate the clinical course of tracheostomized and ventilator-dependent infants with severe BPD. Awareness of this condition in infants with chronic illness will prevent unnecessary investigations since the clinical course is self-limited.
Keywords: Parotitis; Infants; Bronchopulmonary dysplaisa; Case series
| Introduction | ▴Top |
The most common cause of parotitis in infants is bacterial infection [1]. There is limited literature about non-infectious parotitis in infants. Parotitis and other salivary gland inflammation are rare during infancy. The pathogenesis of parotitis in this age group is not fully understood. The majority of cases of parotitis in infants reported in the literature are usually unilateral and suppurative (77%) [1].
In a 2013 review of 44 neonatal patients with parotitis, 33% were former premature infants. Forty-seven percent presented with fever. The majority of these patients were treated with antibiotics [2]. Non-infectious parotitis in preterm infants can occur due to long-term exclusive oro-gastric feeding leading to functional ductal obstruction and local inflammation [3].
Risk factors for parotitis include low birth weight, oral trauma, immune suppression, ductal obstruction, sepsis, malnutrition, prematurity, dehydration and electrolyte imbalance [4].
To our knowledge, there are only five reported cases of non-infectious or aseptic parotitis in the literature in premature infants in the first 6 weeks of life [4]. We report four former extremely premature infants with severe bronchopulmonary dysplasia (BPD) who had tracheostomy for prolonged mechanical ventilation and presented with non-infectious parotitis while still in the neonatal intensive care unit.
| Case Reports | ▴Top |
A retrospective chart review of patients with BPD who developed parotitis was conducted over a 5-year period (January 1, 2013 to December 31, 2017) at a level IV neonatal intensive care unit with a BPD home ventilator program. Parotitis for this study was defined as unilateral or bilateral swelling of the parotid gland on clinical examination and parotid gland inflammation confirmed with a radiological image study.
The charts were reviewed for clinical presentation, imaging studies, surgical and medical treatment, and existing co-morbidities. The study was approved by the Children’s Mercy-Kansas City Institutional Review Board.
During this 5-year period, there were 409 patients with BPD, and 48 (11.7%) of these patients had a tracheostomy (severe BPD). Four patients with severe BPD developed parotitis. All four patients during the episodes of parotitis were on mechanical ventilation through a tracheostomy and feeding through a naso-gastric tube (two patients) or gastrostomy tube (two patients). None of the patients were on any oral feedings. Three of the patients presented with bilateral parotid gland enlargement. One patient presented with unilateral parotid gland enlargement. Two patients had low-grade fever (temperature up to 38°C) at time of presentation. All four patients initially underwent a viral and bacterial infectious work-up including imaging studies, which were negative (Fig. 1 & 2). No suppuration from salivary ducts was present. All four patients had been on a prolonged course of steroid (> 4 weeks) and diuretic (> 4 weeks) therapy for BPD. The demographics and clinical course of patients are summarized in Table 1.
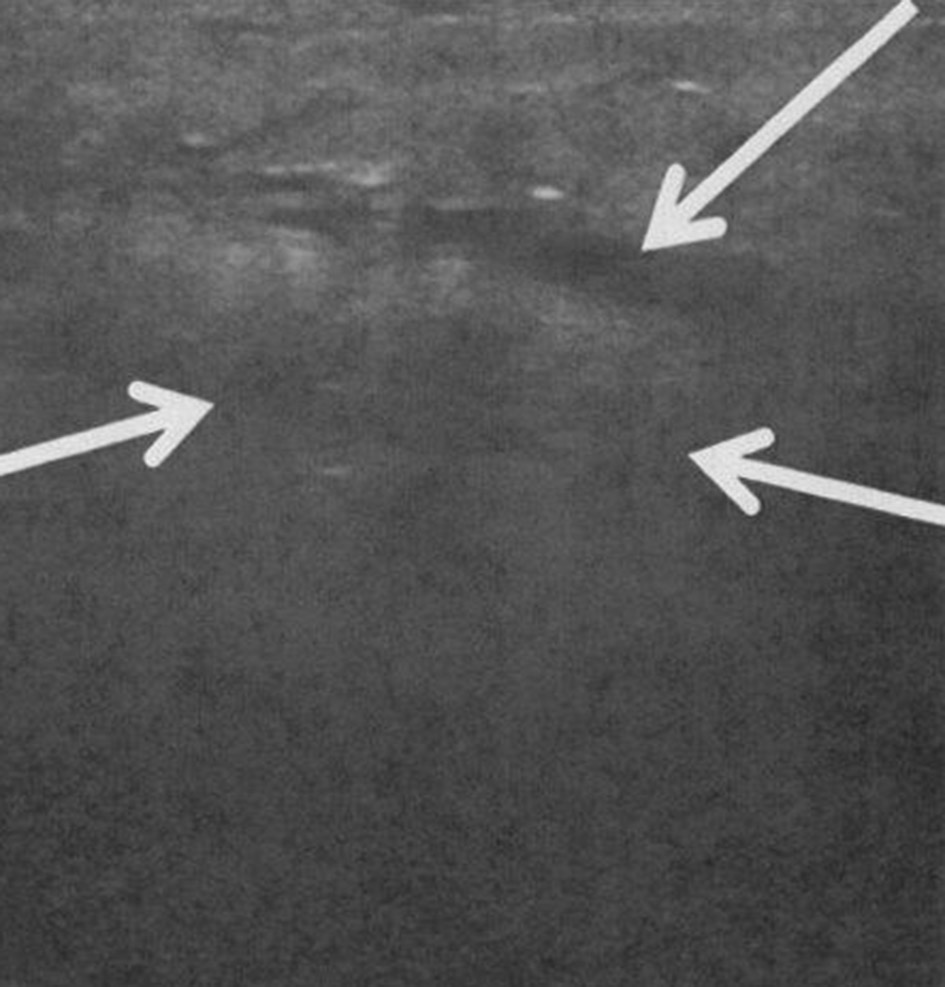 Click for large image | Figure 1. Ultrasound (US) scan of right parotid gland. Longitudinal US image of the right parotid region showing ill-defined tissue with surrounding edema (arrow). No echogenic stones, gas or dilated parotid ducts are seen. |
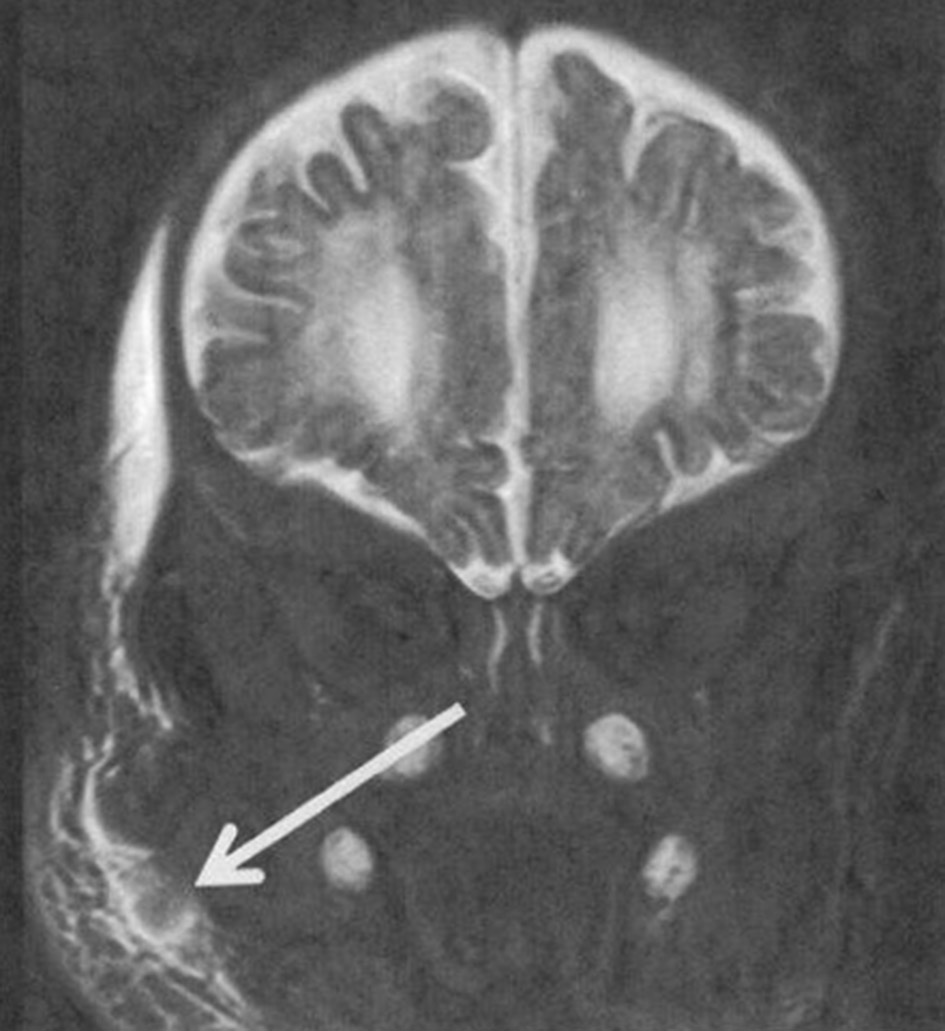 Click for large image | Figure 2. Magnetic resonance imaging of parotid gland. Coronal T2 fat saturated image showing right facial/periparotid edema (arrow). |
 Click to view | Table 1. Patient Characteristics and Clinical Course |
Two of the patients received a course of antibiotics for their initial episode, which did not appear to affect the clinical outcome. Supportive therapy treatment including oral hygiene and allowing small amounts of lemon juice three times a day to assist in salivary gland contraction helped in symptomatic relief. One of the four patients subsequently died of end-stage pulmonary disease.
| Discussion | ▴Top |
Although the most common cause of parotitis during infancy is suppurative, these cases demonstrate non-infectious parotitis occurring in infants with chronic illness. Previous cases of non-infectious parotitis have been reported in preterm infants up to 6 weeks of life [4]. To our knowledge, this is the first case series of non-infectious parotitis in infants with severe BPD.
Multiple factors may play a role in the pathogenesis of acute parotitis in this group of patients with severe BPD. These factors include extreme prematurity, chronic steroid exposure resulting in immune suppression, chronic diuretic use leading to electrolyte imbalance and stasis in the salivary ducts from dehydration, non-oral feeding leading to ductal obstruction, local inflammation due to decreased reflex salivary gland stimulation and saliva production, and poor or abnormal oro-pharyngeal motor function (swallowing).
Awareness of this condition in infants with chronic illness, especially those with any risk factors noted above, is necessary to prevent unnecessary investigations, including viral and bacterial work-up and imaging. The diagnosis of parotitis in these patients is primarily clinical, but ultrasound of the parotid gland may help confirm the diagnosis and rule out abscess formation. Computed tomography scan or magnetic resonance imaging studies may be considered when the diagnosis is in doubt, or to rule out other congenital and inflammatory disorders of the parotid gland.
The differential diagnosis of neonatal and infant parotid gland enlargement includes infectious parotitis, hemangioma, tumors (usually benign), obliteration of Stensen’s duct due to mucous blockage or sialolithiasis, autoimmune conditions (rare in infants) and juvenile recurrent parotitis [5] (also rare in infants). The causes of infectious parotitis are bacterial, and treatment with antibiotics is usually adequate. Only in rare circumstances is drainage of abscess needed [6]. Viral causes include mumps and human immunodeficiency virus and should be considered if the history is suggestive.
The management of non-infectious parotitis is supportive therapy, which includes pain control, external gland massage, adequate hydration and stimulation of oral muscle with salivary duct contraction using small amounts of bitter tasting fluid (lemon juice).
Conclusions
Non-infectious parotitis can complicate the clinical course of tracheostomized and ventilator-dependent infants with severe BPD. Although recurrence of parotitis in this group of patients may not be uncommon, the clinical course appears to be self-limited.
Acknowledgments
Doug Rivard, DO is thanked for providing the images. Kayla Seever and James McBrien are thanked for their assistance with manuscript preparation.
Conflict of Interest
All authors have no conflicts of interest to disclose.
Financial Support
No external funding was secured for this project.
| References | ▴Top |
- Spiegel R, Miron D, Sakran W, Horovitz Y. Acute neonatal suppurative parotitis: case reports and review. Pediatr Infect Dis J. 2004;23(1):76-78.
doi pubmed - Ismail EA, Seoudi TM, Al-Amir M, Al-Esnawy AA. Neonatal suppurative parotitis over the last 4 decades: report of three new cases and review. Pediatr Int. 2013;55(1):60-64.
doi pubmed - Lindgren C, Balihodzic-Lucovic V. Aseptic sialadenitis in preterm infants associated with long-term oro-gastric tube feeding. Eur J Pediatr. 1998;157(12):1014-1016.
doi pubmed - D’Souza JN, Geary C, Mukerji S. Neonatal parotid gland enlargement: Is it suppurative parotitis? A case report. Am J Case Rep. 2012;13(41-43.
- Chitre VV, Premchandra DJ. Recurrent parotitis. Arch Dis Child. 1997;77(4):359-363.
doi - Stong BC, Sipp JA, Sobol SE. Pediatric parotitis: a 5-year review at a tertiary care pediatric institution. Int J Pediatr Otorhinolaryngol. 2006;70(3):541-544.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
