| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website https://www.theijcp.org |
Case Report
Volume 11, Number 3, October 2022, pages 92-97
A Hibernoma of the Neck Complicated With an Abscess
Gill Verstappena, c , Yannick De Bruckerb, Olaf Michela
aDepartment of Otorhinolaryngology - Head and Neck Surgery, Universitair Ziekenhuis Brussel, Vrije Universiteit Brussel, Health Campus, Brussels, Belgium
bDepartment of Radiology, Universitair Ziekenhuis Brussel, Vrije Universiteit Brussel, Health Campus, Brussels, Belgium
cCorresponding Author: Gill Verstappen, Department of Otorhinolaryngology - Head and Neck Surgery, Universitair Ziekenhuis Brussel, Vrije Universiteit Brussel, Health Campus, Brussels, Belgium
Manuscript submitted July 22, 2022, accepted August 20, 2022, published online October 31, 2022
Short title: Hibernoma of the Neck With an Abscess
doi: https://doi.org/10.14740/ijcp496
| Abstract | ▴Top |
A hibernoma is a rare benign soft tissue tumor which may occur in the whole body. In the head and neck region, it occurs only sporadically and is difficult to distinguish clinically and on imaging from malignant tumors. It typically presents as a slow-growing, mobile, non-sensitive mass. Our case report describes an atypical presentation of a hibernoma with sudden onset of swelling in the left neck and dysphagia symptoms in a 16-year-old girl. One week later, a superinfection was noted with discharge of pus. A magnetic resonance imaging (MRI) showed a cystic solid mass, but no definitive diagnosis could be made. Therefore, surgical excision of the mass was performed which proved to be a hibernoma on anatomopathological examination. Whole-body MRI did not show similar lesions in other locations to the head and neck region. A hibernoma should be included in the differential diagnosis in patients presenting with a mass in the head and neck region. It is important to differentiate between benign and malignant tumors since the treatment differs. MRI is the imaging of choice and surgical excision is curative. To our knowledge, this is the first description of a hibernoma with an additional rare abscess formation, making the diagnosis even more difficult.
Keywords: Hibernoma; Soft tissue tumor; Brown adipose tissue; Head; Neck
| Introduction | ▴Top |
A hibernoma is a very rare benign soft tissue tumor, which has been described in the literature since the year 1914 [1]. Only a dozen hibernomas have been reported in the head and neck region since then [2]. Hibernomas originate from the remnant of fetal brown adipose tissue, which is found in the entire body. It has a thermogenesis function in the first life years and spontaneously regresses in general. Thereafter it typically remains asymptomatic unless growth occurs, leading to the development of a soft tissue tumor [3]. Clinically a slow-growing, mobile, non-sensitive mass is usually observed, which is most often located in the thigh, interscapular region and mediastinum but rarely in the head and neck region [4, 5]. We report an unusual case of hibernoma located in the left neck in a teenage girl presenting with dysphagia. The literature and other case reports were reviewed.
| Case Report | ▴Top |
Investigations
A 16-year-old female presented to the emergency room with a painful swelling just anterior to the left sternocleidomastoid muscle and lateral to the thyroid gland that had been present for 2 days. The swelling was well-delineated, soft and painful on palpation. The pain was continuous but more pronounced on mobilization, coughing and swallowing. In addition, dysphagia was present without dysphonia or dyspnea. There was no fever, warmth or redness present. The patient did not present hypotension, fatigue, chills, night sweats or weight loss. The neurological examination was normal on admission. There were normal pulmonary auscultation, smooth and painless abdomen, and no lymphadenopathy. The patient has no significant medical history except for an allergic rhinitis and constipation. There are no hereditary pathologies, nor tumors to withhold. Since she is only 16 years old, she is not yet working.
Diagnosis
The laboratory examination showed an increase in white blood cells (12.1 × 103/mm3) with neutrophilia, hemoglobin 12.0 g/dL, platelets 280 × 103/mm3 and normal C-reactive protein (4.8 mg/L). The thyroid function and kidney function were normal. Epstein-Barr virus (EBV) and cytomegalovirus (CMV) serology were negative. An ultrasound showed an iso- to hypoechogenic solid lesion with a large non-vascularized nodular component. The mass was located lateral to the thyroid gland and inferomedial to the left sternocleidomastoid muscle. The differential diagnosis consisted of a branchial cleft cyst, vascular anomaly, dermoid cyst and paraganglioma. Paracetamol 1 g four times a day and diclofenac retard 75 mg twice daily by mouth were given for the pain.
One week later, the patient returned to the consultation with an increase in symptoms. This was accompanied by pronounced dysphagia and radiating pain to the left arm, but no erythematous skin or fever was present. Amoxiclav 875/125 mg three times a day by mouth was given for 1 week. In the meantime, a magnetic resonance imaging (MRI) was performed, which showed a soft tissue abscess with diffusion restriction and enhancement of the walls. The solid triangular component in the superior part of the lesion had a maximum diameter of 4.2 cm. It was strongly T2 hyperintense, showed no suppression with fat saturation, was isointense on T1 and strongly enhancing after gadolinium administration (Figs. 1 and 2). An ultrasound-guided aspiration was performed on which no cyst could be demonstrated but in which 3 cc of pus could be aspirated. The culture was carried under antibiotics so that no specific bacteria could be isolated. After 1 week of antibiotics, there was improvement of the clinical status of the patient.
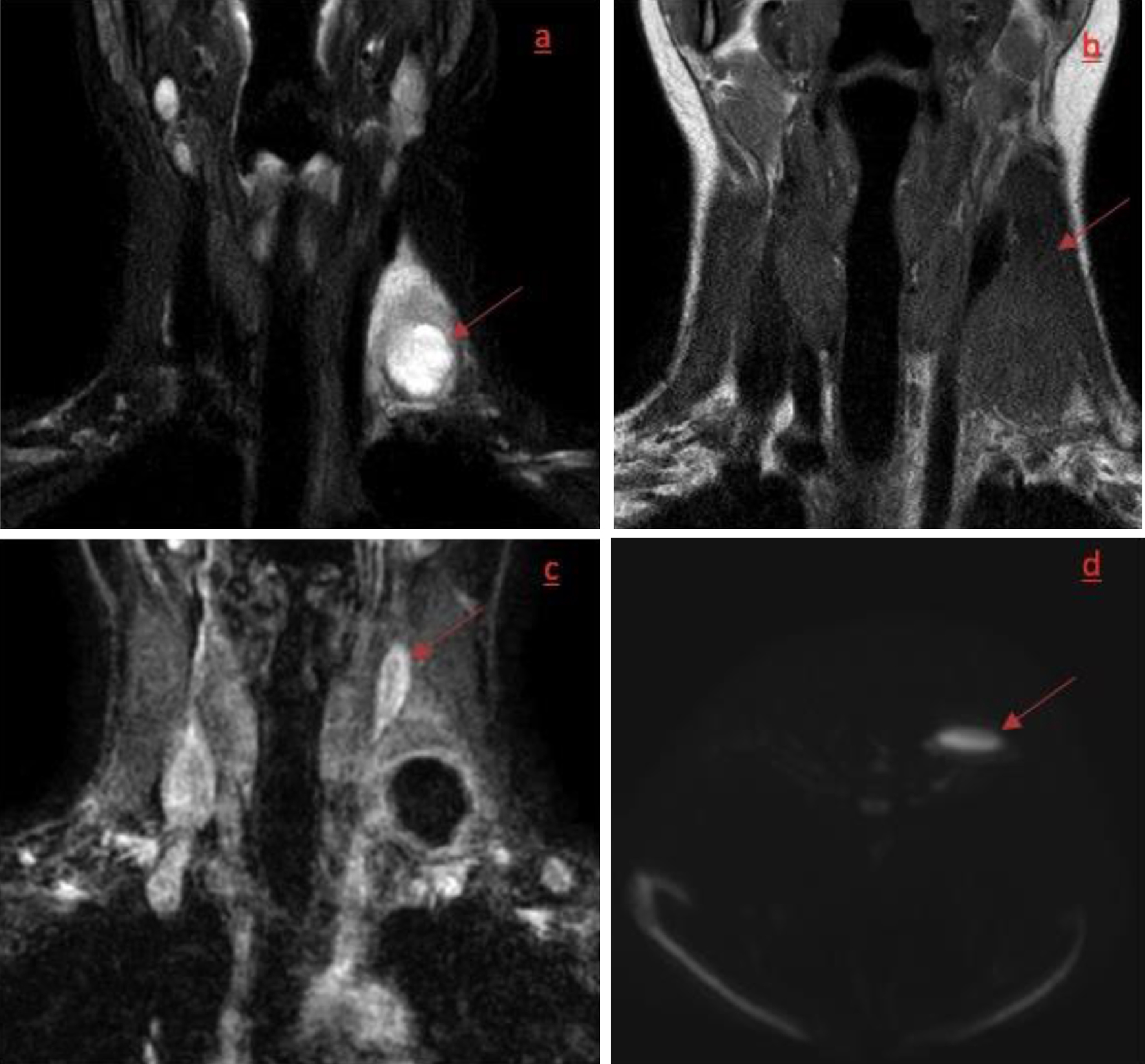 Click for large image | Figure 1. (a, b) Coronal T2-weighted DIXON fat-suppressed image and a coronal T1w image showing a T2 hyperintense and T1 homogeneously hypointense mass in level IV left with central cystic/necrotic formation on T2w. (c, d) Coronal 3DT1 fat-suppressed image after gadolinium showing enhancement of the walls of the central cyst and axial diffusion-weighted image (DWI) showing obvious diffusion restriction, all suggestive for abscess formation in the pre-existing mass. |
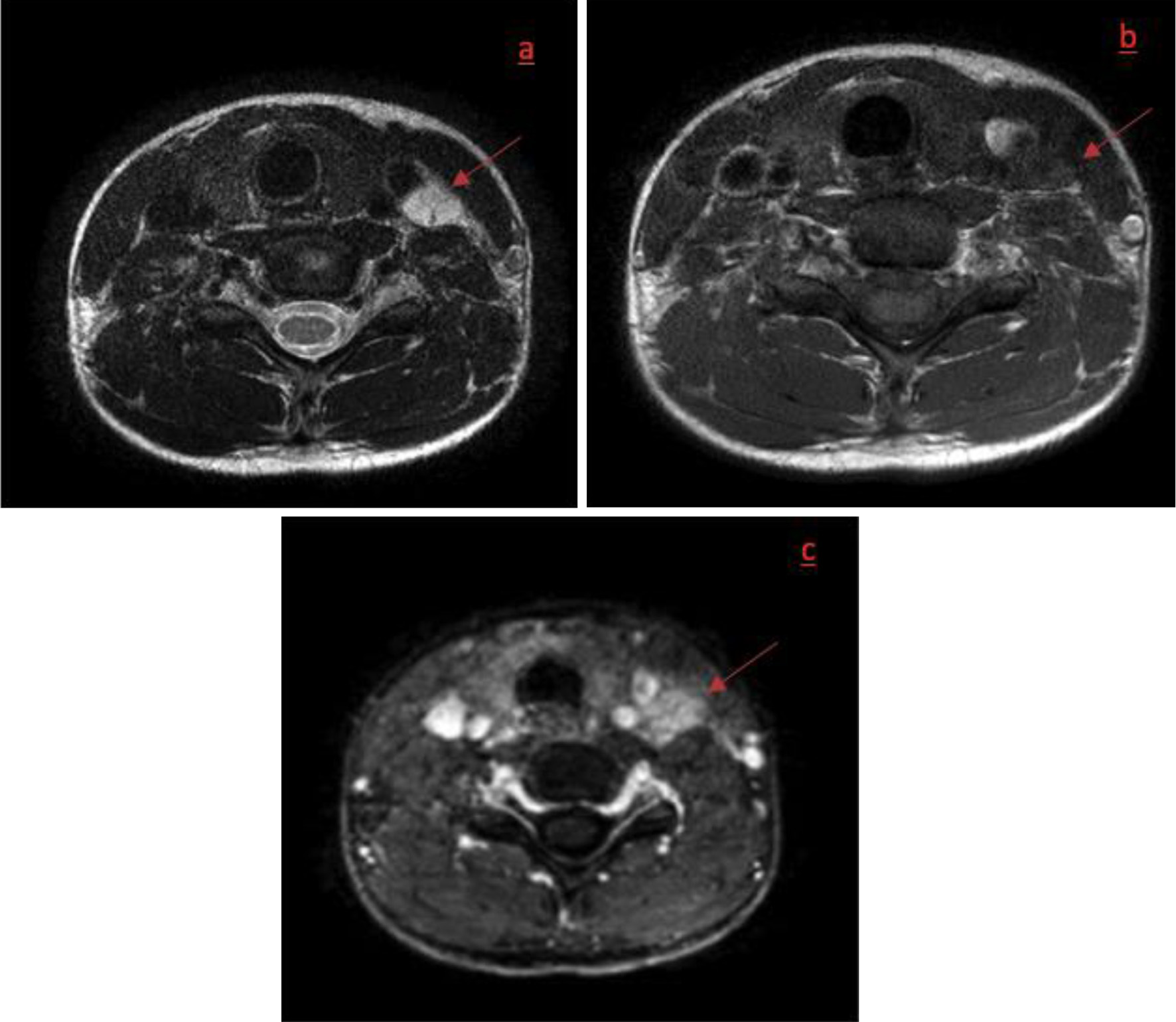 Click for large image | Figure 2. Axial T2w image (a), axial T1w image (b) and axial T1w fat-suppressed image after gadolinium administration (c). Axial section at the upper level of the hibernoma without presence of abscess showing the mass to be T2 hyperintense, isointense to muscle on T1w images and showing a diffuse enhancement after gadolinium. |
Treatment
After informed consent of the patient, the decision was made to surgically remove the mass. The mass at the level of the left neck was removed via a transcervical approach. A well-defined cystic structure around the vena jugularis interna was noted and removed. Anatomopathological examination revealed that a 2.5 × 1.8 × 0.6 cm fragment was removed. The tumor had a soft consistency and a red color.
Follow-up and outcomes
Microscopic examination showed multiple small brown fat cells with multiple small vacuoles on a slightly myxoid background with some reactive lymph nodes. There was no mitotic activity or atypia of nuclei and no signs of malignancy. Several stains to rule out lymphoma were negative (Fig. 3). The tumor was completely removed. The histological picture was consistent with a hibernoma. Comparative genomic hybridization (CGH) shows a simple karyotype, including a homozygous deletion of CDH13 and some partial deletion of 14q, 16q and 17q. No 11q13 rearrangement nor loss of AIP or MEN1.
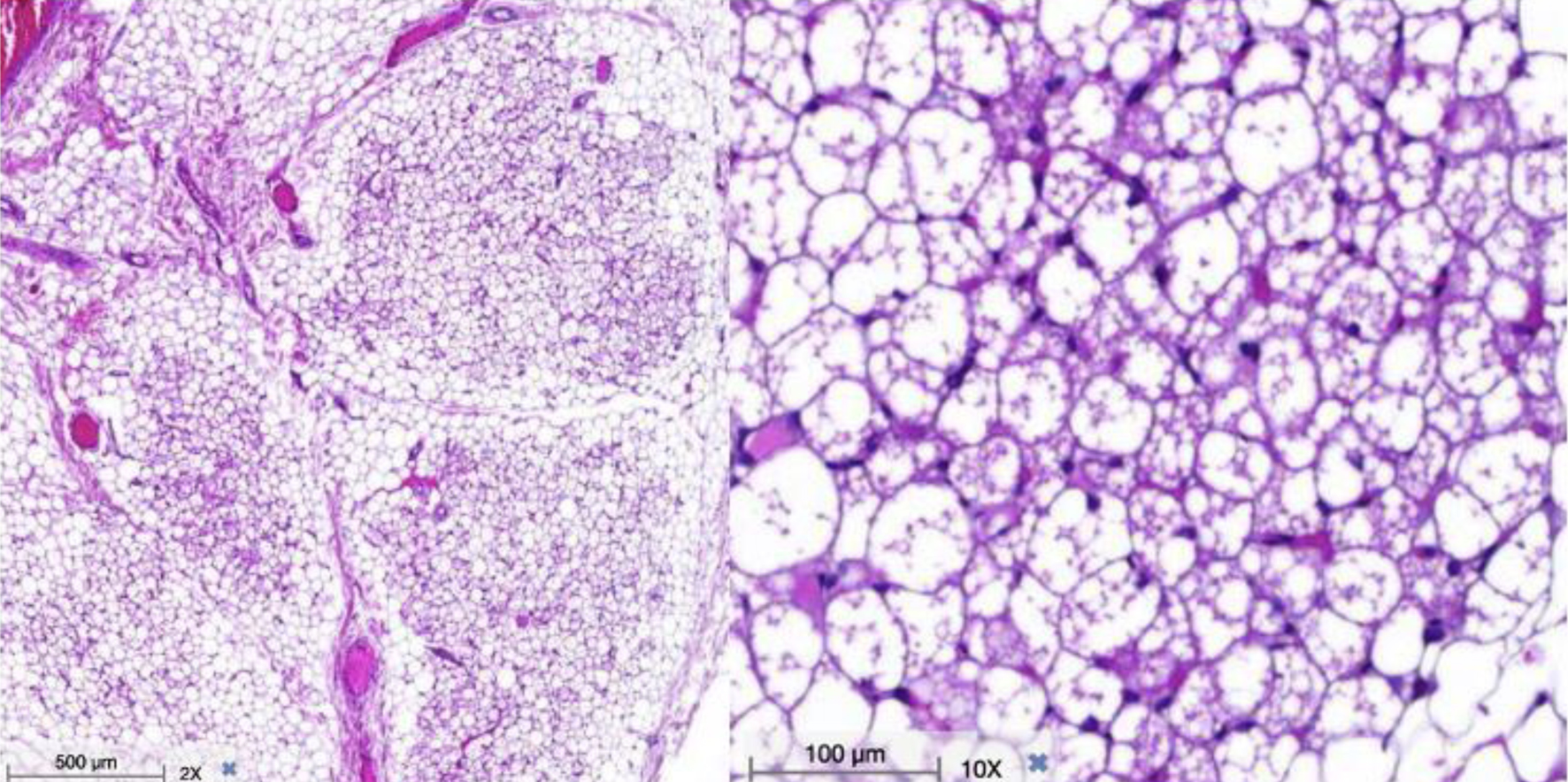 Click for large image | Figure 3. Hematoxylin and eosin stain. Microscopic examination shows multiple small brown fat cells with multiple small vacuoles on a slightly myxoid background (with courtesy from Department of Pathology). |
In the follow-up, a whole-body MRI was performed because a multifocal presentation of hibernoma is not uncommon, and the patient also complained of a palpable swelling in the right thigh. However, in our case, we did not find a synchronous tumor at another site. The patient was satisfied with the treatment and the fact that the entire tumor had been removed. Finally, the follow-up was favorable and no recurrence or new mass was observed clinically up to one and a half years after surgery. Until now, we have no specific cause why a secondary infection occurred.
| Discussion | ▴Top |
A hibernoma is a benign lipid-containing tumor composed of multivacuolated brown adipocytes and originates from the remnants of fetal brown adipose tissue [3]. It was first described by Merkel in 1906 [6], but it was Gery who used the term “hibernoma” in 1914 because of histological similarities to the brown fat of mammals that hibernate [1]. The remnants normally remain asymptomatic unless they grow without identifiable cause and give rise to a soft tissue tumor in various locations in the body [3]. Only a few cases of a hibernoma in the head and neck region are described. Probably it is more prevalent but given the limited knowledge of this tumor, its rarity, and its similarities to asymptomatic lipomas, they are not often diagnosed. However, the latter can transform to a malignant liposarcoma in contrast to a hibernoma which is not known to show malignant transformation.
A hibernoma typically presents as a relatively slow-growing, mobile, non-invasive mass and may cause symptoms by compression of adjacent structures [5]. It is more commonly seen in women with a peak incidence between 30 and 50 years of age [7]. In our case, a hibernoma was diagnosed in a 16-year-old girl with a sudden onset of a mass in the left neck. Unique to this case is the superinfection of the mass with development of an abscess and subsequent associated pain as well as prominent dysphagia symptoms. This was not previously described in the literature to our knowledge. Antibiotics were given after which the symptoms improved.
A hibernoma clinically resembles other benign and malignant tumors so that differential diagnosis should primarily include lipomas and well-differentiated liposarcomas and to a lesser degree fibromas, rhabdomyomas and angiolipomas [8]. A lipoma is often a small, well-circumscribed and poorly vascularized tumor [9].
Imaging is crucial in the attempt to further differentiate diagnosis, but often insufficient to determine malignancy [10]. Signal intensity and homogeneity depend on the ratio of white to brown adipose tissue [11]. Ultrasound can show a well-delineated hyperechogenic mass with hypervascularity and sometimes arteriovenous shunts [12]. In the past, positron emission tomography (PET) was also used as a diagnostic tool since the brown adipose tissue has a significant metabolic activity. However, because of its physiological presence, spots of functional active brown adipose tissue may be present anyway, which causes increased tracer uptake. This form of imaging has been abandoned due to its low specificity [13].
The computed tomography (CT) and MRI examinations typically show a well-delineated mass with signal intensity intermediate between subcutaneous fat and muscle, enhancing after contrast injection. Although they present as brown fat, the imaging characteristics on T1- and T2-weighted images demonstrate high signal intensity but slightly less than that of the subcutaneous fat. On fat suppression sequences, there may be incomplete fat suppression because of the nature and amount of lipids. On MRI, flow voids can be identified. Differentiation of a lipoma can often be done on T1-weighted images since hibernomas appear less intense than neighboring subcutaneous fat, are more vascularized and have larger septae [14]. Unfortunately, the characteristics of a hibernoma described on MRI closely resemble that of a well-differentiated liposarcoma or angiolipoma [15]. Our patient had an additional rare abscess formation, making the diagnosis even more difficult.
A biopsy or excisional biopsy is always necessary for the final diagnosis as medical imaging is inconclusive. Intraoperatively, hibernomas can be recognized macroscopically as a soft rubbery mass that is well-circumscribed, encapsulated, lobulated and often hypervascularized. The color of the mass can vary between light brown to gray and depends on the combination of hypervascularity with abundant mitochondria [11].
Microscopically, brown adipocytes consist of several small droplets with many mitochondria containing iron, which provides the typical macroscopical color [16]. Since this makes it more oxygen-dependent, brown adipose tissue is also often endowed with many capillaries [17]. In addition, mammals also have white adipose tissue in which the adipocytes contain only a single lipid droplet [16]. The typical hibernoma can be described as a pattern of cells with a small round central nucleus containing a large amount of eosinophilic cytoplasm surrounded by a thin cell wall [5, 18]. The cytoplasm consists of multiple small vacuoles and a variable amount of granularity, which typifies the brown fat [5]. Histologically/morphologically, four subtypes or variants are artificially differentiated that actually have no clinical significance: typical, spindle, lipoma-like and myxoid depending on the eosinophilia, configuration and stroma [19].
The treatment of a hibernoma is surgical excision, which is usually sufficient and curative. If completely removed, the chance of relapse is minimal. Excision is the only way to get a final diagnosis of a hibernoma since the clinical picture and imaging are insufficiently specific [7]. Removal may be complicated by the hypervascularity and adhesion of the translucent film to a muscle [18]. No malignant transformations have been described in the literature, nor have metastases been reported [17]. Table 1 gives an overview of the most important characteristics of a hibernoma.
 Click to view | Table 1. Characteristics of Hibernoma |
Learning points
A hibernoma is a rare, benign soft tissue tumor originating in the brown adipose tissue. It is not distinguishable either clinically, nor on imaging from malignant tumors such as a liposarcoma. MRI is the imaging of choice in the differential diagnosis, but a definitive diagnosis can only be made after biopsy or excision. This case report depicts a hibernoma in the head and neck region which is an exceptional location. Even more exceptional is the young age and the sudden onset of symptoms with the existence of an underlying complicating abscess. This was accompanied by prominent dysphagia symptoms, which to our knowledge has not been described before. With complete surgical removal, the risk of recurrence is minimal and - according to the literature search - malignant transformation has never been reported before.
Acknowledgments
Department of Anatomical Pathology University-Hospital Brussels and especially Dr. Sharareh Fadaei who performed the histological examination of the hibernoma.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent for publication was obtained.
Author Contributions
GV did the literature review and analyzed the patient data. YDB performed the radiologic examination. OM did the surgery and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Gery L. In discussion of MF Bonnel's paper. Bull Mem Soc Anat Paris. 1914;89:111-112.
- Dagher W, Fedore L, Wein RO. Hibernoma presenting as an asymptomatic neck mass. Am J Otolaryngol. 2013;34(6):755-756.
doi pubmed - Cannon B, Nedergaard J. Brown adipose tissue: function and physiological significance. Physiol Rev. 2004;84(1):277-359.
doi pubmed - Evers LH, Gebhard M, Lange T, Siemers F, Mailander P. Hibernoma-case report and literature review. Am J Dermatopathol. 2009;31(7):685-686.
doi pubmed - Beals C, Rogers A, Wakely P, Mayerson JL, Scharschmidt TJ. Hibernomas: a single-institution experience and review of literature. Med Oncol. 2014;31(1):769.
doi pubmed - Merkel H. On a pseudolipoma of breast (peculiar fat cell tumor). Beitr Path Anat. 1906;39:152.
- Trujillo O, Cui IH, Malone M, Suurna M. An unusual presentation of a rare benign tumor in the head and neck: A review of hibernomas. Laryngoscope. 2015;125(7):1656-1659.
doi pubmed - Mavrogenis AF, Coll-Mesa L, Drago G, Gambarotti M, Ruggieri P. Hibernomas: clinicopathological features, diagnosis, and treatment of 17 cases. Orthopedics. 2011;34(11):e755-759.
doi - Rodriguez Ruiz A, Saussez S, Demaesschalck T, Lechien JR. Hibernoma: a rare case of adipocytic tumor in head and neck. BMC Ear Nose Throat Disord. 2017;17:13.
doi pubmed - Dursun M, Agayev A, Bakir B, Ozger H, Eralp L, Sirvanci M, Guven K, et al. CT and MR characteristics of hibernoma: six cases. Clin Imaging. 2008;32(1):42-47.
doi pubmed - DeRosa DC, Lim RB, Lin-Hurtubise K, Johnson EA. Symptomatic hibernoma: a rare soft tissue tumor. Hawaii J Med Public Health. 2012;71(12):342-345.
- Hardes J, Scheil-Bertram S, Hartwig E, Gebert C, Gosheger G, Schulte M. Sonographic findings of hibernoma. A report of two cases. J Clin Ultrasound. 2005;33(6):298-301.
doi pubmed - Chatterton BE, Mensforth D, Coventry BJ, Cohen P. Hibernoma: intense uptake seen on Tc-99m tetrofosmin and FDG positron emission tomographic scanning. Clin Nucl Med. 2002;27(5):369-370.
doi pubmed - Papathanassiou ZG, Alberghini M, Taieb S, Errani C, Picci P, Vanel D. Imaging of hibernomas: A retrospective study on twelve cases. Clin Sarcoma Res. 2011;1(1):3.
doi pubmed - Coblentz C, Roberts JT, Fitzgerald E. Hibernoma: a patient examined by CT. Can Assoc Radiol J. 1986;37(2):110-111.
- Enerback S. The origins of brown adipose tissue. N Engl J Med. 2009;360(19):2021-2023.
doi pubmed - Chen CL, Chen WC, Chiang JH, Ho CF. Interscapular hibernoma: case report and literature review. Kaohsiung J Med Sci. 2011;27(8):348-352.
doi pubmed - Salim B, Belkacem C. Hibernoma of the thigh: a report of four cases. J Orthop Surg (Hong Kong). 2014;22(1):118-121.
doi pubmed - Furlong MA, Fanburg-Smith JC, Miettinen M. The morphologic spectrum of hibernoma: a clinicopathologic study of 170 cases. Am J Surg Pathol. 2001;25(6):809-814.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
|
||||||||||||||||||||||||||||||||||



 This journal follows the International Committee of Medical Journal Editors (
This journal follows the International Committee of Medical Journal Editors (